Diabetic Neuropathy Vs. Peripheral Neuropathy: Understanding Nerve Damage
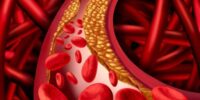
Diabetic neuropathy and peripheral neuropathy are both conditions that involve nerve damage, but they have distinct differences. Diabetic neuropathy refers specifically to nerve damage caused by diabetes, while peripheral neuropathy is a broader term that encompasses nerve damage resulting from various causes.
Understanding the differences between these conditions is crucial for accurate diagnosis and appropriate treatment.
Nerve damage can cause a range of symptoms, including numbness, tingling, and pain in the affected areas. Diabetic neuropathy primarily affects the feet and legs, while peripheral neuropathy can affect any part of the body. The causes of peripheral neuropathy can vary, including factors such as trauma, infections, and autoimmune disorders.
Diagnosing diabetic neuropathy involves evaluating symptoms, conducting physical examinations, and performing nerve function tests. Treatment options for peripheral neuropathy depend on the underlying cause and may involve medication, physical therapy, or surgery. Managing diabetic neuropathy involves maintaining blood sugar levels within a target range, adopting a healthy lifestyle, and managing symptoms effectively.
Preventing nerve damage requires controlling diabetes and managing risk factors such as high blood pressure and high cholesterol. Seeking medical advice and support is essential for proper diagnosis, treatment, and ongoing management of both diabetic and peripheral neuropathy.
Key Takeaways
- Diabetic neuropathy primarily affects the feet and legs, while peripheral neuropathy can affect any part of the body.
- Diagnosing diabetic neuropathy involves evaluating symptoms, physical examinations, and nerve function tests.
- Treatment for peripheral neuropathy depends on the underlying cause and may involve medication, physical therapy, or surgery.
- Managing diabetic neuropathy involves maintaining blood sugar levels, adopting a healthy lifestyle, and managing symptoms.
The Basics of Nerve Damage
Nerve damage, a fundamental aspect of diabetic neuropathy and peripheral neuropathy, is characterized by the impairment or dysfunction of nerves in the body. This condition can result from various causes, such as metabolic disorders, autoimmune diseases, or physical trauma.
Nerve damage disrupts the transmission of signals between the brain and the rest of the body, leading to a range of symptoms including pain, numbness, tingling, and muscle weakness. Diabetic neuropathy specifically refers to nerve damage caused by chronically high blood sugar levels in individuals with diabetes. On the other hand, peripheral neuropathy refers to nerve damage that occurs outside the brain and spinal cord.
Both conditions can have a significant impact on a person’s quality of life, affecting their mobility, balance, and overall well-being. Understanding the basics of nerve damage is crucial for effective management and treatment of these conditions.
Symptoms of Diabetic Neuropathy
Pain, numbness, and tingling sensations are commonly experienced by individuals with diabetic neuropathy. These symptoms typically begin in the feet and legs and may gradually progress to the hands and arms. Other symptoms include muscle weakness, loss of coordination, and difficulty walking. The severity of symptoms can vary, ranging from mild discomfort to excruciating pain, which can significantly impact a person’s quality of life.
To further illustrate the impact of diabetic neuropathy, consider the following sub-lists:
-
Physical Symptoms:
- Burning or stabbing pain
- Sensitivity to touch or temperature changes
- Muscle cramps or spasms
- Loss of reflexes
-
Functional Limitations:
- Difficulty in maintaining balance
- Impaired mobility and coordination
- Increased risk of falls and injuries
- Challenges in performing daily activities such as grasping objects or buttoning clothes.
Understanding these symptoms is crucial in the early detection and management of diabetic neuropathy, ultimately improving the overall well-being of individuals affected by this condition.
Causes of Peripheral Neuropathy
One key aspect to consider when exploring the causes of peripheral neuropathy is the potential impact of underlying medical conditions on nerve function. There are various medical conditions that can lead to peripheral neuropathy, including diabetes, autoimmune diseases, infections, and traumatic injuries. Diabetes is one of the most common causes of peripheral neuropathy, as high blood sugar levels can damage the nerves over time. Autoimmune diseases, such as rheumatoid arthritis and lupus, can also contribute to nerve damage by causing inflammation in the body. Infections, such as Lyme disease and HIV/AIDS, can directly affect the nerves and lead to peripheral neuropathy. Additionally, traumatic injuries, such as car accidents or falls, can result in nerve damage. Understanding the underlying medical conditions is crucial in diagnosing and managing peripheral neuropathy effectively.
| Medical Condition | Impact on Nerve Function | |||
|---|---|---|---|---|
| Diabetes | Damages nerves over time | |||
| Autoimmune diseases | Causes inflammation in the body | |||
| Infections | Directly affects the nerves | |||
| Traumatic injuries | Results in nerve damage | Neurodegenerative diseases | Gradually deteriorates nerve function | |
| ————————— | ————————————- |
Diagnosing Diabetic Neuropathy
The diagnosis of diabetic neuropathy involves assessing a patient’s medical history, conducting a physical examination, and performing specific tests to evaluate nerve function and identify any potential complications.
Medical history assessment entails gathering information about the patient’s symptoms, their duration, and any underlying medical conditions that may contribute to nerve damage.
A physical examination may involve testing the patient’s reflexes, muscle strength, and sensitivity to touch, temperature, and vibration.
Specific tests used to diagnose diabetic neuropathy include nerve conduction studies, which assess the speed and strength of nerve signals, and electromyography, which evaluates muscle activity.
Additionally, autonomic testing may be performed to assess the functioning of the autonomic nerves that control involuntary bodily functions.
These diagnostic procedures aid in determining the presence and extent of diabetic neuropathy, allowing for appropriate management and treatment strategies.
Treatment Options for Peripheral Neuropathy
Treatment options for peripheral neuropathy include a combination of medications, lifestyle modifications, and alternative therapies. The goal of treatment is to manage symptoms, slow down the progression of the disease, and improve the patient’s quality of life. Here are several options that can be considered:
-
Medications: Several medications may be prescribed to relieve pain and manage other symptoms associated with peripheral neuropathy. These may include pain relievers, anti-seizure medications, and antidepressants.
-
Lifestyle modifications: Making certain lifestyle changes can also help alleviate symptoms. This may include maintaining a healthy weight, engaging in regular exercise, avoiding alcohol and tobacco, and managing stress levels.
-
Alternative therapies: Certain alternative therapies, such as acupuncture, biofeedback, and physical therapy, may provide relief from peripheral neuropathy symptoms. These therapies aim to stimulate nerves, improve blood circulation, and reduce pain and discomfort.
-
Nutritional supplements: Some nutritional supplements, such as alpha-lipoic acid and vitamin B12, may be recommended to help improve nerve function and reduce symptoms.
It is important for individuals with peripheral neuropathy to work closely with their healthcare provider to determine the most suitable treatment plan based on their specific needs and symptoms.
Managing Diabetic Neuropathy
Managing diabetic neuropathy involves implementing a comprehensive approach that combines medication, lifestyle modifications, and alternative therapies to effectively alleviate symptoms and enhance the overall well-being of individuals with this condition.
Medications commonly prescribed for diabetic neuropathy include anticonvulsants, antidepressants, and opioids. These medications aim to reduce pain and discomfort by targeting the underlying nerve damage.
Additionally, lifestyle modifications play a crucial role in managing diabetic neuropathy. This includes maintaining blood glucose levels within a target range, adopting a healthy diet, engaging in regular physical activity, and quitting smoking. These lifestyle changes help to reduce inflammation, improve blood flow, and promote nerve health.
Alternative therapies, such as acupuncture, massage, and relaxation techniques, may also provide some relief for individuals with diabetic neuropathy.
It is important for individuals to work closely with healthcare professionals to develop a personalized treatment plan that addresses their specific needs and goals.
Preventing Nerve Damage
Managing Diabetic Neuropathy involves various strategies aimed at alleviating symptoms and slowing the progression of nerve damage. However, prevention is always better than cure. Therefore, it is crucial to focus on Preventing Nerve Damage in individuals with diabetes.
By maintaining optimal blood sugar levels through regular monitoring and adhering to a well-balanced diet, the risk of developing nerve damage can be significantly reduced. Additionally, implementing a regular exercise routine and managing weight effectively can help enhance blood circulation, thereby minimizing the chances of nerve damage. Quitting smoking and limiting alcohol consumption are also essential in preventing further damage to the nerves.
Furthermore, individuals should practice proper foot care, including inspecting feet daily, keeping them clean and moisturized, and wearing appropriate footwear to prevent injuries and infections that may lead to nerve damage. By diligently following these preventive measures, individuals can take proactive steps in safeguarding their nerves and overall well-being.
Seeking Medical Advice and Support
Seeking medical advice and support is crucial for individuals with diabetes who may be experiencing symptoms related to nerve damage, as healthcare professionals can provide guidance and personalized recommendations to help manage the condition effectively.
When experiencing symptoms such as numbness, tingling, or pain in the extremities, it is important to consult a healthcare provider for a proper diagnosis. They can evaluate the individual’s medical history, perform physical examinations, and order tests to determine the cause and severity of the nerve damage.
Based on the findings, healthcare professionals can develop an individualized treatment plan that may include medications to manage pain, lifestyle modifications to control blood sugar levels, and referrals to specialists if needed.
Regular follow-up visits with healthcare professionals are also important to monitor the progression of the condition and make any necessary adjustments to the treatment plan.
Seeking medical advice and support ensures that individuals with diabetic neuropathy or peripheral neuropathy receive appropriate care and support to minimize the impact of nerve damage on their quality of life.
Frequently Asked Questions
Are there any alternative treatments available for peripheral neuropathy?
Alternative treatments for peripheral neuropathy include medications such as neuropathic pain relievers, antidepressants, and anticonvulsants. Additionally, non-pharmacological approaches such as physical therapy, acupuncture, and transcutaneous electrical nerve stimulation (TENS) may also be beneficial.
How long does it take to diagnose diabetic neuropathy?
The diagnosis of diabetic neuropathy can vary depending on the individual and the specific symptoms present. It typically involves a thorough medical history, physical examination, and nerve function tests.
Can peripheral neuropathy be reversed or cured?
Peripheral neuropathy cannot be fully reversed or cured, but its symptoms can be managed and progression can be slowed down with proper treatment. Treatment may include medication, physical therapy, and lifestyle changes.
Are there any specific exercises or physical therapy that can help manage diabetic neuropathy?
There are specific exercises and physical therapy options that can help manage diabetic neuropathy. These interventions aim to improve strength, balance, and flexibility, reduce pain, and improve overall quality of life for individuals with diabetic neuropathy.
Are there any specific risk factors for developing peripheral neuropathy?
Specific risk factors for developing peripheral neuropathy include diabetes, alcohol abuse, certain medications, autoimmune diseases, infections, kidney and liver diseases, and exposure to toxins. Other factors include age, family history, and certain vitamin deficiencies.