Reproduction And Fertility Explained
Reproduction and fertility are fundamental aspects of human life, yet they are complex processes that are often misunderstood. Understanding the anatomy and function of the male and female reproductive systems, the hormonal processes involved in the menstrual cycle, and the factors that affect fertility is critical for individuals and couples who are planning to start a family. This article provides a comprehensive overview of reproduction and fertility, including the various disorders that can affect these processes and the treatment options available.
The male reproductive system includes the testes, epididymis, vas deferens, seminal vesicles, prostate gland, and urethra. The testes produce sperm, which are stored in the epididymis until ejaculation. The vas deferens transports the sperm to the urethra, where they are mixed with seminal fluid produced by the seminal vesicles and prostate gland.
In women, the reproductive system includes the ovaries, fallopian tubes, uterus, cervix, and vagina. The ovaries produce and release eggs, which travel down the fallopian tubes towards the uterus. If fertilization occurs, the fertilized egg implants in the lining of the uterus, where it develops into a fetus. Understanding the anatomy and function of these reproductive organs is essential for understanding how reproduction and fertility work.
Key Takeaways
- Age is a crucial factor affecting fertility, while lifestyle factors such as smoking, excessive alcohol consumption, and drug use can harm reproductive function and decrease chances of conception.
- Certain health conditions, such as PCOS and endometriosis, can affect fertility. Reproductive disorders can also be caused by genetic abnormalities, hormonal imbalances, and infections.
- ARTs are medical techniques used to facilitate conception, with IVF, ICSI, and IUI being common ART procedures. However, ARTs have risks and ethical concerns.
- Maintaining a healthy lifestyle and seeking medical treatment if experiencing fertility issues is important. A healthy weight, diet, and exercise can improve fertility outcomes, while reducing stress and avoiding tobacco and alcohol use can increase chances of achieving a healthy pregnancy.
The Male Reproductive System: Anatomy and Function
The male reproductive system is comprised of various organs, including the testes, epididymis, vas deferens, seminal vesicles, prostate gland, and urethra, which work together to produce and transport sperm.
The testes, located in the scrotum, are responsible for producing sperm and testosterone.
The epididymis, located above and behind each testicle, stores and matures the sperm.
The vas deferens transports the sperm from the epididymis to the seminal vesicles, where they are combined with semen before ejaculation.
The prostate gland, located just below the bladder, produces a fluid that nourishes and protects the sperm.
The urethra, which runs through the penis, is responsible for ejaculating the semen during sexual intercourse.
The male reproductive system is also responsible for producing hormones that are essential for sexual development and function.
Testosterone, produced by the testes, is responsible for the development of male sex organs, deepening of the voice, and growth of body hair.
It also plays a role in sexual desire and fertility.
The male reproductive system is a complex and intricate system that plays a vital role in human reproduction and sexual function.
Understanding its anatomy and function is important for maintaining overall health and well-being.
The Female Reproductive System: Anatomy and Function
One of the complex physiological systems in female mammals is the reproductive system, which includes the ovaries, fallopian tubes, uterus, and vagina. The ovaries are two small, almond-shaped glands located on either side of the uterus, and they produce and release eggs.
The fallopian tubes are two thin tubes that extend from the ovaries to the uterus, where they provide a pathway for the egg to travel to meet the sperm. The uterus is a muscular organ that can expand to accommodate a growing fetus during pregnancy, and it contracts during childbirth to expel the baby.
The vagina is the muscular canal that connects the cervix, the lower part of the uterus, to the outside of the body, and it is the site of sexual intercourse and the birth canal.
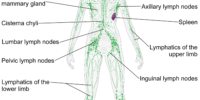
The female reproductive system is regulated by hormones, including estrogen and progesterone, which are produced by the ovaries. The menstrual cycle is a complex series of events that occurs in the female reproductive system and is controlled by these hormones.
It begins with the release of an egg from one of the ovaries and ends with the shedding of the uterine lining if the egg is not fertilized. Fertilization occurs when a sperm meets an egg in the fallopian tube, and the resulting embryo implants in the uterine lining, leading to pregnancy.
The female reproductive system is essential for the continuation of the species and plays a central role in human reproduction and fertility.
The Menstrual Cycle: Hormones and Processes Involved
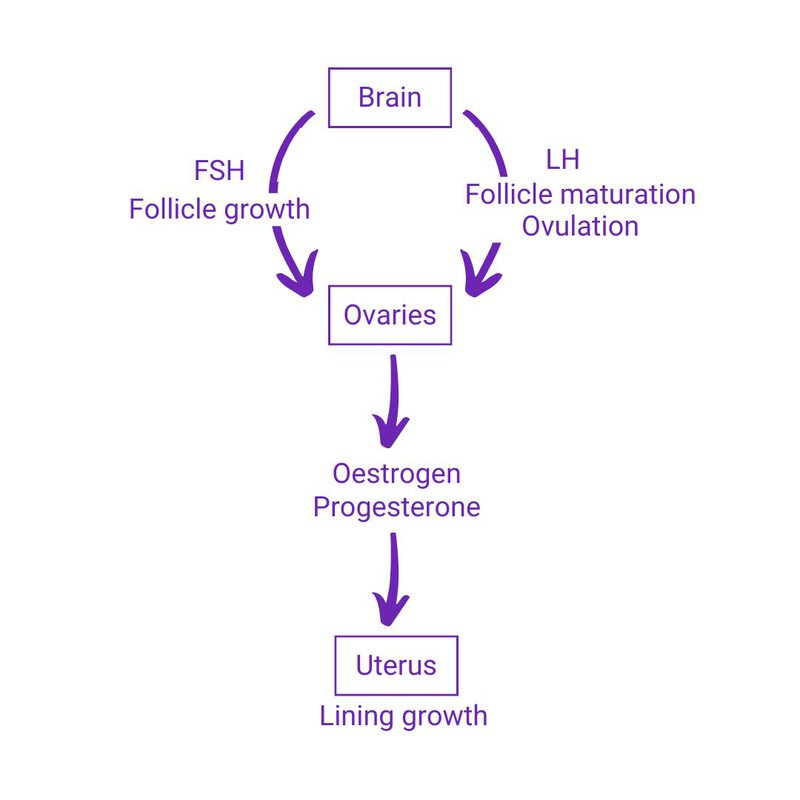
Understanding the hormonal fluctuations and physiological processes involved in the menstrual cycle is crucial for women’s health and reproductive planning. The menstrual cycle is a complex process that involves the interaction between various hormones, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone. These hormones work together to regulate the growth and development of the follicle, ovulation, and the preparation of the uterus for implantation.
The menstrual cycle can be divided into two phases: the follicular phase and the luteal phase. During the follicular phase, FSH stimulates the growth and development of the follicle, which contains the egg. As the follicle grows, it produces estrogen, which causes the thickening of the uterine lining. When estrogen levels reach a certain threshold, it triggers a surge in LH, which causes the follicle to rupture and release the egg. This process is called ovulation.
After ovulation, the luteal phase begins, and the ruptured follicle forms the corpus luteum, which produces progesterone. Progesterone prepares the uterus for implantation by thickening the uterine lining and suppressing ovulation. If the egg is not fertilized, the corpus luteum degenerates, and progesterone levels drop, which triggers the shedding of the uterine lining and the onset of a new menstrual cycle.
Conception: From Fertilization to Implantation
Conception is a complex process involving the fusion of a sperm and an egg, resulting in the formation of a zygote that undergoes a series of cell divisions before implantation in the uterus. This process usually occurs in the Fallopian tube, where the egg is released from the ovary and travels towards the uterus. The sperm, which are deposited in the vagina during sexual intercourse, swim towards the egg and penetrate its outer layer. Once a single sperm has successfully penetrated the egg, a chemical reaction occurs that prevents other sperm from entering. This process, called fertilization, marks the beginning of a new life.
After fertilization, the zygote undergoes a series of cell divisions as it travels towards the uterus. By the time it reaches the uterus, it has developed into a cluster of cells called a blastocyst. The blastocyst then implants into the lining of the uterus, where it will continue to grow and develop over the next nine months. The implantation process is facilitated by the hormone progesterone, which is produced by the corpus luteum after ovulation. Implantation usually occurs between six and ten days after fertilization and is accompanied by symptoms such as mild cramping and spotting.
Factors Affecting Fertility: Age, Lifestyle, and Health
Various factors, including age, lifestyle, and health, can significantly impact an individual’s ability to conceive and carry a pregnancy to term.
Age is one of the most important factors affecting fertility. Women are born with a finite number of eggs, and the quality and quantity of these eggs decline as they age. As women approach their mid-30s and beyond, their chances of getting pregnant naturally decrease significantly. Men’s fertility also declines with age, although the decline is more gradual than in women.
Lifestyle factors can also affect fertility. Smoking, excessive alcohol consumption, and drug use can all harm reproductive function and decrease the chances of conception. Similarly, being overweight or underweight can impact fertility by disrupting hormone levels.
Lastly, certain health conditions, such as polycystic ovary syndrome (PCOS) and endometriosis, can also affect fertility. It is important for individuals to maintain a healthy lifestyle and seek medical treatment if they are experiencing fertility issues.
Reproductive Disorders: Causes and Treatment Options
As mentioned in the previous subtopic, several factors can affect fertility, including age, lifestyle, and health. However, even individuals who maintain a healthy lifestyle and are within their reproductive years may experience reproductive disorders that can affect their ability to conceive. These disorders can be caused by various factors, such as genetic abnormalities, hormonal imbalances, and infections.
Reproductive disorders can manifest in different ways, such as menstrual irregularities, ovulatory dysfunction, and male or female infertility. Fortunately, several treatment options are available to address these issues, ranging from medication to surgical interventions. In this subtopic, we will explore the common reproductive disorders, their causes, and the available treatment options. To help clarify the information, a table summarizing the disorders, causes, and treatment options will be provided.
Fertility Treatments: Assisted Reproductive Technologies
Assisted reproductive technologies (ARTs) have revolutionized the field of reproductive medicine. These procedures involve the use of medical techniques to manipulate and facilitate conception, particularly in cases where traditional methods have failed. The most common ART procedures include in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and intrauterine insemination (IUI).
IVF is the most well-known and widely used ART procedure. It involves the fertilization of an egg outside the body and the subsequent transfer of the embryo into the uterus.
ICSI, on the other hand, involves the direct injection of a single sperm into an egg, which is then implanted into the uterus. IUI is a less invasive procedure that involves the placement of sperm into the uterus through a catheter during ovulation.
While ARTs have been successful in helping many couples achieve pregnancy, they are not without risks and ethical concerns. It is important for individuals to discuss their options with a qualified healthcare provider and make informed decisions about their reproductive health.
Family Planning: Tips for Improving Reproductive Health
To optimize reproductive health, individuals can implement various lifestyle changes and strategies. Maintaining a healthy weight is one of the most important factors for both men and women. Overweight or obese individuals are at a higher risk for fertility problems and complications during pregnancy.
A healthy diet and regular exercise can help to achieve and maintain a healthy weight, which in turn can improve fertility outcomes. Reducing stress is also important for reproductive health. Chronic stress can have negative effects on the reproductive system, leading to hormonal imbalances and reduced fertility.
Engaging in stress-reducing activities such as yoga, meditation, or regular exercise can help to improve overall well-being and reduce stress levels. Additionally, avoiding smoking and excessive alcohol consumption can also improve reproductive health outcomes. Tobacco and alcohol use have been linked to reduced fertility in both men and women, as well as increased risk for pregnancy complications.
Making these lifestyle changes and strategies a priority can help individuals improve their reproductive health and increase their chances of achieving a healthy pregnancy.
Conclusion
In conclusion, reproduction and fertility are complex topics that involve various anatomical and physiological processes.
The male and female reproductive systems have distinct structures and functions that allow for the production and transport of gametes.
The menstrual cycle is a complex process regulated by hormones, which prepares the uterus for pregnancy.
Conception occurs when a sperm fertilizes an egg, leading to the formation of a zygote that implants in the uterine wall.
Factors such as age, lifestyle, and health can affect fertility, and reproductive disorders can arise due to various causes.
Fortunately, there are several treatment options available, including assisted reproductive technologies, for individuals struggling with infertility.
Family planning is crucial for improving reproductive health, and individuals can take steps to maintain optimal reproductive function.
Overall, understanding reproductive and fertility processes can help individuals make informed decisions about their health and family planning goals.