The Connection Between Blood Sugar And Diabetes
Diabetes is a chronic condition that affects millions of people worldwide. It is characterized by high blood sugar levels, which can lead to a range of complications if left unmanaged.
Blood sugar, also known as glucose, is a vital component of the body’s energy supply. It comes from the food we eat and is transported through the bloodstream to various cells and tissues where it is used for energy.
The connection between blood sugar and diabetes is complex and multifaceted. Understanding how blood sugar works and the role of insulin in its regulation is crucial for managing diabetes.
This article will explore the different types of diabetes, their causes, symptoms and complications of high blood sugar, and the various strategies for managing blood sugar levels. It will also discuss the latest research and treatment options for diabetes.
Key Takeaways
- Blood sugar is a vital component in the energy supply of the body and plays a crucial role in diabetes management.
- Diabetes is a chronic condition that affects millions worldwide and can lead to severe and life-threatening complications.
- Type 1 diabetes is an autoimmune disease that destroys insulin-producing cells, while Type 2 diabetes is a metabolic disorder that causes insulin resistance or insufficient production.
- Lifestyle changes, medication, and monitoring are essential for diabetes management, and promising areas of research include stem cell therapy and smart insulin.
What is Blood Sugar and How Does it Work?
Blood sugar, also known as glucose, is a crucial source of energy for the body’s cells. It is mainly obtained from the food we eat and is transported through the bloodstream to the cells where it is used for energy.
However, glucose levels in the blood need to be regulated to prevent them from becoming too high or too low, as both conditions can have harmful effects on the body.
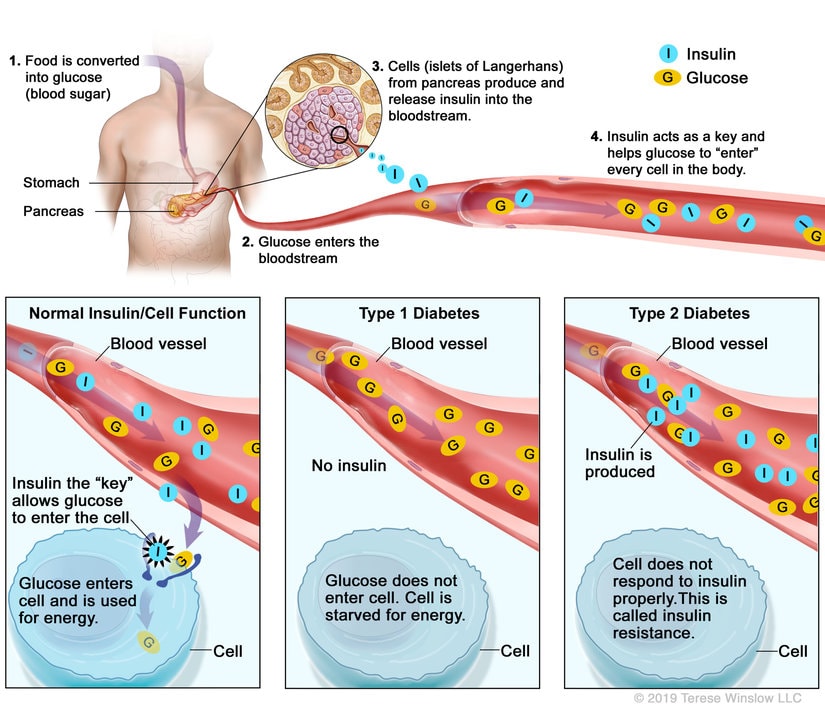
The body uses insulin and glucagon, two hormones produced by the pancreas, to regulate blood sugar levels. Insulin helps to lower blood sugar levels by promoting the uptake of glucose by cells and the liver, where it is stored as glycogen. Glucagon, on the other hand, raises blood sugar levels by promoting the breakdown of glycogen in the liver and the release of glucose into the bloodstream.
The balance between these two hormones is essential to maintain blood sugar levels within a healthy range. Understanding how blood sugar is regulated is crucial in understanding the development and management of diabetes, a condition in which the body is unable to regulate blood sugar levels effectively.
The Role of Insulin in Blood Sugar Regulation
Insulin, a hormone secreted by the pancreas, plays a crucial role in the maintenance of normal blood glucose levels in the body. It regulates the metabolism of carbohydrates, fats, and proteins by promoting the uptake of glucose from the bloodstream into the cells, where it is used for energy or stored for future use.
Insulin also inhibits the release of glucose from the liver and stimulates the conversion of excess glucose into glycogen, a storage form of glucose in the liver and muscles. To further emphasize the importance of insulin in blood sugar regulation, here are four key functions of insulin in the body:
- Increases glucose uptake in muscle and fat cells
- Inhibits glucose production in the liver
- Promotes glycogen synthesis in the liver and muscles
- Enhances the conversion of glucose to fat for storage in adipose tissue
Without insulin, the body cannot use glucose effectively, resulting in high blood sugar levels and eventually leading to diabetes. Therefore, insulin therapy is a cornerstone of diabetes management and is used to replace or supplement the body’s natural insulin production in people with type 1 diabetes or advanced type 2 diabetes.
Types of Diabetes and Their Causes
There are various types of diabetes, each with different underlying causes, which lead to disruptions in the body’s ability to regulate its blood sugar levels. The two main types of diabetes are type 1 and type 2 diabetes. Type 1 diabetes is an autoimmune disease in which the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. This results in a lack of insulin production, which leads to high blood sugar levels. Type 1 diabetes is usually diagnosed in children and young adults, and it accounts for about 5-10% of all diabetes cases.
On the other hand, type 2 diabetes is a metabolic disorder in which the body becomes resistant to insulin or does not produce enough insulin to maintain normal blood sugar levels. This type of diabetes is more common and accounts for about 90-95% of all diabetes cases. Type 2 diabetes is often associated with lifestyle factors such as obesity, physical inactivity, and poor diet. Other risk factors for type 2 diabetes include age, family history, and certain medical conditions such as high blood pressure and high cholesterol. Understanding the different types of diabetes and their causes is important for effective management and treatment of the disease.
| Type of Diabetes | Underlying Cause | ||
|---|---|---|---|
| Type 1 | Autoimmune destruction of insulin-producing cells in the pancreas | ||
| Type 2 | Insulin resistance or insufficient insulin production due to lifestyle factors and/or genetic predisposition | ||
| Gestational | Hormonal changes during pregnancy that affect insulin sensitivity | ||
| LADA | A slow-developing form of type 1 diabetes that occurs in adults | ||
| MODY | A rare genetic form of diabetes that is inherited in an autosomal dominant pattern | and is caused by mutations in specific genes that affect insulin production and secretion. |
Symptoms and Complications of High Blood Sugar
The symptoms and potential complications of elevated glucose levels can have a significant impact on individuals with diabetes. One of the most common symptoms of high blood sugar is frequent urination, which occurs as the body tries to remove excess glucose from the bloodstream.
Increased thirst and hunger are also common, as the body tries to compensate for the high glucose levels. Other symptoms include fatigue, blurred vision, and slow-healing wounds.
Complications of high blood sugar can be severe and life-threatening. Over time, elevated glucose levels can damage blood vessels and nerves, leading to cardiovascular disease, kidney disease, neuropathy, and blindness. In extreme cases, high blood sugar can cause diabetic ketoacidosis, a condition that occurs when the body breaks down fat for energy instead of glucose, resulting in a buildup of toxic acids in the bloodstream.
It is crucial for individuals with diabetes to monitor their blood sugar levels regularly and seek medical attention if they experience any symptoms or complications.
Diagnosis and Monitoring of Diabetes
Monitoring and diagnosing diabetes involves regular testing of blood glucose levels, as well as measuring glycosylated hemoglobin (A1C) levels, which provides an average of blood glucose levels over the past two to three months. The American Diabetes Association recommends that people with diabetes monitor their blood glucose levels at least four times a day, or as directed by their healthcare provider. This can be done using a blood glucose meter, which requires a small drop of blood from a fingerstick.
In addition to self-monitoring of blood glucose, healthcare providers may also order A1C testing every three to six months to assess how well a person’s diabetes is being managed. The target A1C level for people with diabetes is typically less than 7%, although individual targets may vary based on age, duration of diabetes, and the presence of other health conditions. Other tests that may be used to diagnose or monitor diabetes include fasting blood glucose, oral glucose tolerance test, and random blood glucose. Regular monitoring and testing is crucial for managing diabetes and preventing complications.
| Test Name | Normal Range | Diabetes Range |
|---|---|---|
| Fasting Blood Glucose | 70-99 mg/dL | ≥126 mg/dL |
| Oral Glucose Tolerance Test | <140 mg/dL | ≥200 mg/dL |
| Random Blood Glucose | <140 mg/dL | ≥200 mg/dL |
| A1C | <5.7% | ≥6.5% |
Table 1: Normal and diabetes ranges for common diabetes tests.
Lifestyle Changes for Managing Blood Sugar
Managing blood sugar levels in individuals with diabetes requires making significant lifestyle changes. These changes include adopting a healthy diet, engaging in regular physical activity, monitoring blood sugar levels, and taking medications as prescribed.
A healthy diet for individuals with diabetes should consist of foods that are low in sugar, fat, and salt, and high in fiber and nutrients. This means avoiding sugary and processed foods, and instead opting for whole grains, fruits, vegetables, lean protein, and healthy fats.
Physical activity is also essential for managing blood sugar levels in individuals with diabetes. Regular exercise helps to lower blood sugar levels, improve insulin sensitivity, and maintain a healthy weight. It is recommended that individuals with diabetes engage in moderate-intensity aerobic exercise for at least 150 minutes per week, in addition to resistance training at least two days per week.
Monitoring blood sugar levels is another important aspect of managing diabetes. This involves regularly checking blood sugar levels at home using a glucose meter and keeping a record of the results.
Finally, taking medications as prescribed by a healthcare provider is crucial for managing blood sugar levels in individuals with diabetes. This may include medications such as insulin or oral medications that help to lower blood sugar levels.
Overall, adopting a healthy lifestyle and following a comprehensive diabetes management plan can help individuals with diabetes to effectively manage their blood sugar levels and prevent complications associated with the condition.
Medications for Controlling Blood Sugar
One crucial aspect of successfully managing diabetes involves utilizing medications to regulate glucose levels and prevent long-term complications. There are several classes of medications available on the market that work by targeting different mechanisms in the body.
For example, metformin is a commonly prescribed medication that works by reducing glucose production in the liver and improving insulin sensitivity. Sulfonylureas, on the other hand, stimulate the pancreas to release more insulin and are effective at lowering blood sugar levels. Other medications such as thiazolidinediones, DPP-4 inhibitors, GLP-1 receptor agonists, and SGLT-2 inhibitors also have different mechanisms of action and can be used in combination with other medications to achieve optimal glucose control.
However, it is important to note that medications alone are not enough to manage diabetes. Lifestyle modifications such as a healthy diet, regular exercise, and weight management are also essential to achieving good glucose control.
In addition, it is crucial for individuals with diabetes to work closely with their healthcare providers to monitor their blood sugar levels and adjust medications as needed. With proper medication management and adherence to lifestyle changes, individuals with diabetes can prevent long-term complications and improve their overall health and wellbeing.
Future Directions in Diabetes Research and Treatment
With the advancements in technology and research, the future of diabetes treatment and management looks promising. Scientists are exploring new avenues to develop innovative treatments and therapies to help individuals with diabetes live a better life. Researchers are investigating various approaches to cure diabetes at its root cause, which would eliminate the need for lifelong medication.
One promising area of research is stem cell therapy. It involves using stem cells to regenerate beta cells in the pancreas, which are responsible for producing insulin. The goal is to create a functioning pancreas that can regulate blood sugar levels, thereby eliminating the need for insulin injections. Another area of research is the development of smart insulin, which can detect blood sugar levels and release insulin as needed. This would make the management of diabetes more convenient for patients and reduce the risk of hypoglycemia.
| Treatment/Therapy | Advantages | Disadvantages |
|---|---|---|
| Stem Cell Therapy | Potential cure for diabetes | High cost and limited availability |
| Smart Insulin | Convenient and reduces risk of hypoglycemia | Still in development and may not be effective for all patients |
In addition to these innovative treatments, researchers are also exploring the use of technology to improve diabetes management. Continuous glucose monitoring (CGM) systems and artificial pancreas systems are two examples of technology that can help individuals with diabetes manage their blood sugar levels more effectively. CGM systems use sensors to monitor blood sugar levels throughout the day, while artificial pancreas systems automate insulin delivery based on CGM data.
Overall, the future of diabetes treatment and management looks bright with various promising research directions. Continued advancements in technology and research will undoubtedly lead to improved therapies and treatments that can make a significant impact on the lives of individuals with diabetes.
Conclusion
In conclusion, blood sugar regulation is a complex process that involves several hormones and organs in the body.
Diabetes is a disease that results from a disruption in this process, leading to high blood sugar levels.
There are two main types of diabetes, each with its own causes and risk factors.
Symptoms of high blood sugar include frequent urination, increased thirst, and blurred vision.
Timely diagnosis and management of diabetes are critical to prevent complications such as heart disease, kidney failure, and nerve damage.
Lifestyle changes such as a healthy diet, exercise, and weight management can help manage blood sugar levels, along with medications such as insulin and oral antidiabetic drugs.
With ongoing research and advancements in treatment options, there is hope for better management and prevention of diabetes in the future.