The Role Of Blood Clotting In Wound Healing
The human body has a remarkable ability to repair itself after sustaining an injury. One of the most critical steps in this process is blood clotting, which occurs when blood vessels are damaged or broken.
Blood clotting is a complex process that involves a series of biochemical events that ultimately lead to the formation of a clot, which stops the flow of blood and provides a physical barrier to prevent further bleeding.
In addition to its role in controlling bleeding, blood clotting also plays a crucial role in wound healing.
Understanding the process of blood clotting and its role in wound healing is essential for medical professionals who treat patients with injuries. In this article, we will explore the mechanisms of blood clotting, the importance of blood clotting in wound healing, and the different factors that can affect blood clotting.
We will also discuss the various disorders and abnormalities associated with blood clotting, as well as the future research directions in this field.
By understanding the complex interplay between blood clotting and wound healing, we can develop better strategies for preventing and treating injuries.
Key Takeaways
- Blood clotting is critical for tissue repair and wound healing as it prevents excessive blood loss, provides a physical barrier, and triggers the release of growth factors.
- Platelets play a crucial role in the coagulation process by adhering to the injured vessel wall, becoming activated, and releasing chemicals that initiate clot formation.
- Disruptions to the balance of pro-coagulant and anti-coagulant factors can lead to abnormal clotting or bleeding disorders such as hemophilia and thrombophilia.
- Advancements in regenerative medicine, including the development of novel drugs and therapies, exploration of the role of platelets and fibrin in wound healing, and the use of biomaterials and tissue engineering, hold great promise for the development of new therapies.
The Process of Blood Clotting
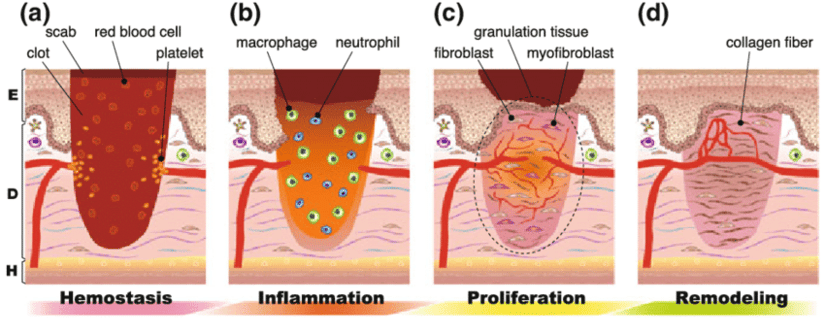
The process of blood clotting, also known as hemostasis, involves a complex sequence of events that results in the formation of a stable clot at the site of injury.
The process is initiated when blood vessels are damaged, leading to the exposure of the underlying collagen.
Platelets, which are small, disc-shaped cells in the blood, are then activated and begin to adhere to the exposed collagen.
This leads to the formation of a platelet plug, which helps to temporarily stop bleeding.
Next, the clotting cascade is initiated, which involves a series of reactions that ultimately result in the conversion of fibrinogen to fibrin.
Fibrin is a protein that forms a mesh-like structure around the platelet plug, further stabilizing the clot.
The clotting cascade is a complex process involving a number of different factors, including enzymes, proteins, and platelets.
Once the clot has formed, it helps to prevent further bleeding and provides a scaffold for the migration of cells involved in wound healing.
The Importance of Blood Clotting in Wound Healing
A crucial aspect in the process of tissue repair is the formation of a protective barrier that prevents the entry of harmful pathogens and promotes cellular proliferation. This is where blood clotting plays a critical role in wound healing. The process of blood clotting, or coagulation, involves the activation of platelets and the deposition of fibrin to form a clot.
This clot acts as a temporary seal over the injury, preventing blood loss and reducing the risk of infection. The importance of blood clotting in wound healing cannot be overstated.
Here are three key reasons why blood clotting is crucial in the process of tissue repair:
- Blood clotting prevents excessive blood loss, which can be life-threatening in the case of severe injuries.
- The clot provides a physical barrier to protect the wound from further damage and infection.
- The clotting process triggers the release of growth factors, which promote cellular proliferation and tissue regeneration. This is a critical step in the healing process, as it allows new tissue to form and replace the damaged tissue.
The Role of Platelets in Blood Clotting
Platelets are small, anucleate cell fragments that circulate in the blood and play a crucial role in the coagulation process. When there is damage to a blood vessel, platelets are the first responders that arrive at the site of the injury. They adhere to the injured vessel wall and become activated, releasing a cascade of chemicals that initiate the formation of a blood clot. The clotting process involves a series of complex interactions between platelets, coagulation factors, and other blood components. Together, they work to form a fibrin mesh that reinforces the platelet plug and stabilizes the clot.
Platelet function is regulated by a delicate balance of pro-coagulant and anti-coagulant factors. Disruptions to this balance can lead to abnormal clotting or bleeding disorders. For example, genetic mutations that affect platelet function can result in conditions such as von Willebrand disease or Bernard-Soulier syndrome, which are characterized by defective platelet adhesion or aggregation. On the other hand, medications that interfere with platelet function, such as aspirin or clopidogrel, are commonly used to prevent thrombotic events in patients with cardiovascular disease. Understanding the role of platelets in blood clotting is essential for developing effective treatments for these conditions.
| Pro-Coagulant Factors | Anti-Coagulant Factors |
|---|---|
| Platelets | Protein C |
| Coagulation Factors | Protein S |
| Fibrinogen | Antithrombin III |
| Thrombin | Tissue Factor Pathway Inhibitor |
Table: Pro-coagulant and anti-coagulant factors involved in blood clotting. The balance of these factors is crucial for maintaining normal hemostasis.
The Formation of Fibrin Clots
Interactions between coagulation factors and fibrinogen lead to the formation of stable fibrin clots, which are essential for preventing excessive bleeding. The formation of fibrin clots involves a complex process that occurs in response to tissue damage.
This process begins with the activation of platelets, which adhere to the site of injury and release chemicals that promote the activation of clotting factors. The subsequent activation of clotting factors and fibrinogen leads to the formation of a fibrin meshwork that stabilizes the platelet plug.
The formation of fibrin clots also involves several regulatory mechanisms that prevent the clot from becoming too large and obstructing blood flow. These mechanisms include the activation of anticoagulant factors and the removal of excess fibrin by fibrinolysis.
Overall, the formation of fibrin clots plays a critical role in wound healing by preventing excessive bleeding and promoting the formation of a stable clot that facilitates tissue repair.
The Inflammatory Response and Blood Clotting
The inflammatory response is an essential component of the body’s defense mechanism against tissue damage and infection. This process initiates a series of events that aim to limit the spread of pathogens and repair any damaged tissues.
One of the primary functions of the inflammatory response is to activate blood clotting, which prevents excessive bleeding and seals off the damaged area. The initial step in this process involves the activation of platelets, which aggregate at the site of injury and adhere to the exposed collagen in the damaged vessel wall. This results in the formation of a temporary platelet plug that serves to stop any further blood loss.
Following this, a series of complex biochemical reactions occur that lead to the formation of a fibrin clot. These reactions involve the activation of various clotting factors, which convert fibrinogen into fibrin, a protein that forms a mesh-like structure that reinforces the platelet plug.
This fibrin clot acts as a scaffold for the migration and proliferation of cells involved in the subsequent stages of wound healing. The inflammatory response and blood clotting are therefore intricately linked, with both processes playing crucial roles in the body’s defense mechanisms and the restoration of damaged tissues.
The Role of Blood Clotting in Preventing Infection
Infection prevention is a vital function of the body’s defense mechanisms, and an important aspect of this is the formation of a mesh-like protein structure that reinforces the temporary plug at the site of injury. This structure is known as a fibrin clot, which is formed by the activation of a complex cascade of proteins known as the coagulation pathway.
The clot acts as a physical barrier that prevents bacteria and other pathogens from entering the wound, and it also provides a framework for the migration of immune cells that are responsible for clearing out any invading microorganisms.
To further enhance infection prevention, the clotting process also stimulates the production of antimicrobial peptides and cytokines, which are molecules that help to fight off infections. Antimicrobial peptides are small proteins that have a broad-spectrum antimicrobial activity, meaning that they can kill a wide range of microorganisms, including bacteria, fungi, and viruses.
Cytokines, on the other hand, are signaling molecules that help to coordinate the immune response by recruiting immune cells to the site of infection and activating them to destroy any invading pathogens. Together, the fibrin clot, antimicrobial peptides, and cytokines form a formidable defense mechanism that helps to prevent infections and promote wound healing.
Disorders and Abnormalities of Blood Clotting
Disorders and abnormalities related to coagulation can lead to various health complications and require appropriate medical attention.
One of the most common disorders of blood clotting is hemophilia, a genetic disorder that affects the ability of the blood to clot properly. Hemophilia is characterized by recurrent bleeding episodes, which can range from mild to severe. Individuals with severe hemophilia may experience spontaneous bleeding into their joints, which can cause chronic joint pain and damage. Hemophilia is usually diagnosed in childhood, and treatment involves the administration of clotting factor replacement therapy to prevent bleeding episodes.
Another disorder of blood clotting is thrombophilia, a condition where the blood has an increased tendency to form clots. Thrombophilia can be caused by genetic mutations that affect clotting factors or by acquired conditions such as obesity, pregnancy, or prolonged immobility. The most serious complication of thrombophilia is the formation of blood clots in the deep veins of the legs, which can break loose and travel to the lungs, causing a life-threatening condition called pulmonary embolism.
Treatment for thrombophilia may include anticoagulant medications, which prevent the formation of blood clots, or thrombolytic therapy, which dissolves existing blood clots. Early detection and appropriate management of disorders of blood clotting are essential for preventing complications and improving the quality of life of affected individuals.
Future Research Directions in Blood Clotting and Wound Healing
Advancements in the field of regenerative medicine are paving the way for new methods to improve tissue repair and regeneration, which could have significant implications for the treatment of injuries and wound healing.
The role of blood clotting in wound healing has been extensively studied, and current research is focused on developing new therapies that can enhance this process.
Here are some of the future research directions in blood clotting and wound healing:
- Development of novel drugs and therapies that can target specific components of the blood clotting cascade to enhance wound healing.
- Exploration of the role of platelets, which are essential for blood clotting, in the wound healing process and development of therapies that can modulate their function.
- Investigation of the role of fibrin, a protein that is essential for blood clotting, in wound healing and development of therapies that can enhance its function.
- Use of biomaterials and tissue engineering approaches to develop new wound dressings that can promote blood clotting, tissue regeneration, and wound healing.
- Development of non-invasive imaging techniques to monitor blood clotting and wound healing in real-time, which can help in the development of new therapies and interventions.
Overall, these research directions hold great promise for the development of new therapies that can enhance the role of blood clotting in wound healing and improve outcomes for patients with injuries and wounds.
Conclusion
In conclusion, blood clotting is a crucial component of wound healing. The process involves a complex sequence of events that ultimately leads to the formation of a fibrin clot and the prevention of excessive blood loss.
Platelets play a critical role in initiating and maintaining the clotting process, while the inflammatory response helps to promote healing and prevent infection.
However, disorders and abnormalities of blood clotting can have serious consequences and may result in excessive bleeding or clot formation. Future research in this area will be important for developing new treatments and therapies to improve wound healing outcomes and prevent complications.
Overall, a better understanding of the role of blood clotting in wound healing has the potential to improve patient outcomes and reduce the burden of disease.