The Science Behind Blood Types: What Makes Them Unique?
Blood is a vital fluid that circulates through our bodies, delivering essential nutrients and oxygen to our cells. However, not all blood is the same. Blood types are determined by the presence or absence of specific antigens on the surface of red blood cells. This diversity in blood types has significant implications for medical treatment, as incompatible blood transfusions can lead to life-threatening complications.
In this article, we will explore the science behind blood types, including the history of blood typing, the different blood group systems, and the importance of blood typing in medical treatment. The study of blood types has a long and fascinating history, dating back to the early 20th century. The discovery of blood types and the development of blood typing techniques revolutionized the field of medicine, allowing for safer blood transfusions and more effective medical treatments.
Understanding the science behind blood types is crucial for medical professionals, as it enables them to provide the best possible care for their patients. So, what makes blood types unique, and how do they impact medical treatment? Let’s delve into the science behind blood types and find out.
Key Takeaways
- Blood types are determined by specific antigens on red blood cells, which can cause life-threatening complications if incompatible transfusions occur.
- ABO blood group system has 4 types: A, B, AB, and O, with type O being the universal donor and AB being the universal recipient.
- Rh factor also plays a crucial role in transfusions and pregnancies, and inheritance of blood types is determined by genes from both parents.
- Blood typing is crucial for medical professionals in transfusions, transplants, and pregnancy, and advancements in blood typing technology have the potential to revolutionize transfusions and emergency situations.
The History of Blood Typing
The historical origins of blood typing can be traced back to the early 20th century, when scientists began to investigate the existence of different blood groups and their potential significance in medical procedures.
In 1901, Karl Landsteiner, an Austrian biologist, discovered the ABO blood group system, which is still widely used today. Through his experiments, he found that the blood of individuals could be classified as either A, B, AB or O, based on the presence or absence of specific antigens on the surface of red blood cells.
Following Landsteiner’s discovery, other scientists continued to study blood typing and its potential applications. In the 1920s, researchers identified the Rh blood group system, which is based on the presence or absence of the Rh factor on red blood cells.
This system is particularly important in transfusions and pregnancy, as Rh-negative mothers can produce antibodies against Rh-positive fetal blood, which can result in hemolytic disease of the newborn.
Today, blood typing is an essential part of medical practice, allowing for safe and effective transfusions, organ transplants and other medical procedures.
Understanding Antigens and Antibodies
Antigens and antibodies play a crucial role in determining blood type compatibility and can help prevent adverse reactions during blood transfusions. Antigens are molecules found on the surface of red blood cells that are recognized by the immune system as either ‘self’or ‘non-self.’The presence or absence of certain antigens determines blood type.
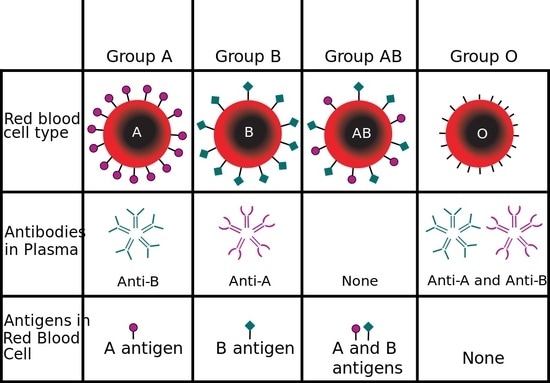
For example, blood type A has A antigens on its red blood cells, blood type B has B antigens, blood type AB has both A and B antigens, and blood type O has neither A nor B antigens.
Antibodies, on the other hand, are proteins produced by the immune system that recognize and bind to foreign antigens. In the case of blood transfusions, the recipient’s immune system can produce antibodies against the donor’s red blood cells if they perceive them as ‘non-self.’
This can result in an adverse reaction, such as fever, chills, and possibly even organ damage. To prevent this, blood transfusions must be carefully matched for blood type and screened for any antibodies that may react with the donor’s blood.
The importance of antigen-antibody reactions in blood transfusions cannot be overstated. A single incompatible transfusion can result in severe and potentially life-threatening reactions. Understanding blood type compatibility can help prevent these adverse events and save lives. The discovery of blood types and the development of safe blood transfusion practices have revolutionized medicine and saved countless lives.
ABO Blood Group System
One of the most well-known and widely studied blood group systems is the ABO system, which is based on the presence or absence of A and B antigens on the surface of red blood cells. The ABO system has four main blood types: A, B, AB, and O. These blood types are determined by the presence or absence of A and B antigens and antibodies in the blood. Blood type A has only the A antigen on the surface of red blood cells and has anti-B antibodies in the blood plasma. Blood type B has only the B antigen on the surface of red blood cells and has anti-A antibodies in the blood plasma. Blood type AB has both A and B antigens on the surface of red blood cells and no antibodies in the blood plasma. Lastly, blood type O has neither A nor B antigens on the surface of red blood cells and has both anti-A and anti-B antibodies in the blood plasma.
The ABO system plays a crucial role in blood transfusion and organ transplantation. Blood type O is considered the universal donor because it has neither A nor B antigens on the surface of red blood cells, making it safe for transfusion to individuals with any blood type. On the other hand, blood type AB is considered the universal recipient because it has both A and B antigens on the surface of red blood cells, making it possible to receive blood from any blood type. Additionally, the ABO system is important in determining paternity and forensic investigations. By analyzing the blood types of individuals, it is possible to rule out potential fathers or identify suspects in criminal investigations.
Rh Factor and Other Blood Group Systems
Rh factor is a protein that is found on the surface of red blood cells and is a major blood group system that plays a crucial role in blood transfusions and pregnancies.
The Rh factor was first discovered in the mid-20th century and was named after the Rhesus monkey, which was used in the initial experiments.
The Rh factor is either present (+) or absent (-) on the surface of red blood cells, and individuals who have the Rh factor are classified as Rh-positive, while those who lack the Rh factor are classified as Rh-negative.
The Rh factor is important in blood transfusions because individuals who are Rh-negative can produce antibodies against Rh-positive blood if they are exposed to it.
This can lead to a severe reaction if they receive Rh-positive blood in a transfusion.
Additionally, the Rh factor is crucial in pregnancy because if a mother is Rh-negative and the fetus is Rh-positive, there is a risk of hemolytic disease of the newborn, which can lead to severe anemia and even death.
However, this risk can be prevented through the administration of Rh immunoglobulin to the mother during pregnancy.
Overall, the Rh factor is an important blood group system that plays a critical role in blood transfusions and pregnancies and highlights the importance of blood typing in medical settings.
Inheriting Blood Types
The inheritance of blood types is a fascinating aspect of genetics that can reveal important information about an individual’s ancestry and potential health risks. Blood types are inherited through a combination of genes from both parents.
The ABO blood group system, for instance, is determined by the presence or absence of two antigens (A and B) on the surface of red blood cells. People with blood type A have the A antigen, those with blood type B have the B antigen, and those with blood type AB have both A and B antigens. People with blood type O, on the other hand, do not have either A or B antigens.
The Rh factor, another blood group system, is determined by the presence or absence of a specific protein (the Rh factor) on the surface of red blood cells. People who have the protein are Rh positive, while those who do not are Rh negative. Inheriting Rh factor is also determined by genes from both parents.
Understanding the inheritance of blood types is important for blood transfusions, organ transplants, and pregnancy, as incompatible blood types can lead to serious complications.
Importance of Blood Typing in Medical Treatment
Understanding the inheritance patterns of blood types is crucial in ensuring safe and effective medical treatment.
Blood typing is a process of identifying the blood group of an individual. It involves testing the blood sample for the presence of antigens and antibodies. Antigens are proteins found on the surface of red blood cells, while antibodies are proteins produced by the immune system in response to foreign antigens.
Blood typing is important in medical treatment because it helps to determine the compatibility of blood transfusions and organ transplants. Blood transfusions are life-saving procedures that involve transferring blood from one person to another. However, if the wrong blood type is transfused, it can lead to a severe reaction that can cause organ failure or even death. Therefore, it is essential to match the blood type of the donor and recipient before any transfusion.
Similarly, organ transplants require matching the blood type of the donor and the recipient to prevent rejection of the transplanted organ. Blood typing is also important in determining the risk of disease transmission through blood products. For example, people with blood type AB are universal recipients, but they are also at a higher risk of contracting certain infectious diseases such as hepatitis B and HIV.
Blood Type Compatibility for Transfusions
Blood type compatibility is crucial in ensuring safe and effective blood transfusions. When a person receives a blood transfusion, their body can potentially reject the foreign blood cells, leading to a range of complications. To avoid this, medical professionals must carefully match the blood type of the donor and the recipient.
Here are some factors that determine blood type compatibility:
- A, B, and O antigens: These antigens are present on the surface of red blood cells and help the immune system recognize foreign substances.
- Type A blood has A antigens, type B blood has B antigens, and type AB blood has both A and B antigens.
- Type O blood has neither A nor B antigens.
- Rh factor: Another important factor in blood type compatibility is the presence or absence of the Rh factor.
- Those with the Rh factor are Rh-positive, while those without it are Rh-negative.
- A person with Rh-negative blood can receive Rh-negative or Rh-positive blood, but a person with Rh-positive blood can only receive Rh-positive blood.
Other factors that can affect blood type compatibility include antibodies, which are produced by the immune system in response to foreign antigens. Medical professionals must also consider the donor’s blood type, the amount of blood being transfused, and the recipient’s overall health status before performing a blood transfusion.
Blood type compatibility is an essential consideration in any blood transfusion. By carefully matching the blood type of the donor and recipient, medical professionals can help ensure a safe and successful procedure. Understanding the factors that determine blood type compatibility can help patients and their healthcare providers make informed decisions about their treatment options.
Future Developments in Blood Typing Technology
Advancements in blood typing technology have the potential to revolutionize the way blood transfusions are performed, with the development of more accurate and efficient methods for identifying blood types.
One of the most promising areas of research in this field is the development of point-of-care testing devices that can quickly and accurately determine blood type at the patient’s bedside. These devices would be particularly useful in emergency situations, where time is of the essence, and accurate blood typing can be the difference between life and death.
Another area of research is the development of non-invasive blood typing methods that do not require a blood sample. These methods include using saliva, urine, or even breath samples to determine blood type. While these methods are still in the early stages of development, they have the potential to greatly reduce the discomfort and inconvenience associated with traditional blood typing methods.
Additionally, they could make it easier and more convenient for people to donate blood, as they would not need to have their blood drawn to determine their blood type.
Conclusion
In conclusion, blood typing plays a critical role in medical treatment. The ABO blood group system and the Rh factor are the most widely used methods of blood typing, but there are other systems as well. The inheritance of blood types is complex, and knowing one’s blood type can help with health management and transfusion compatibility.
Due to advancements in technology, blood typing has become more accurate and efficient. New technologies such as genotyping and next-generation sequencing have improved the ability to identify rare blood types and screen for potential transfusion reactions.
As research continues, the science behind blood typing is likely to become even more sophisticated, making it an increasingly indispensable tool for clinicians. Ultimately, understanding the science behind blood types is crucial for improving patient outcomes and advancing the field of medicine.








