What Are Anticoagulants And How Do They Prevent Blood Clots?
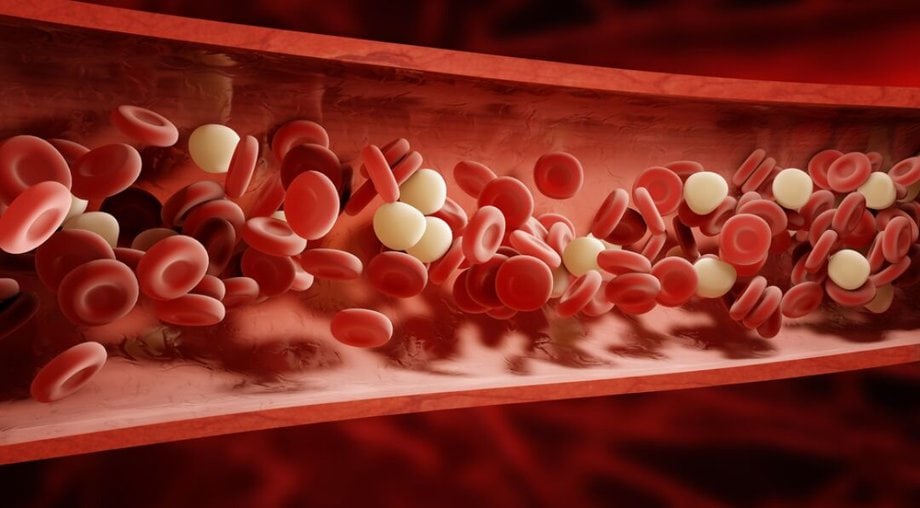
Anticoagulants play a crucial role in preventing the formation of blood clots, a condition that can potentially lead to life-threatening complications. This article aims to provide a comprehensive understanding of what anticoagulants are and how they function to prevent blood clot formation. The mechanisms of action by which anticoagulants work in the body will be examined, exploring the specific processes and pathways involved in inhibiting clot formation.
Additionally, the various types of anticoagulants available and their specific uses in different clinical scenarios will be discussed. Furthermore, this article will delve into the common conditions and disorders that are treated with anticoagulants. The potential side effects and risks associated with anticoagulant therapy will also be explored, along with strategies for monitoring and managing anticoagulant therapy.
Finally, future developments and advancements in anticoagulant treatment will be considered. By addressing these key aspects, this article aims to provide a comprehensive overview of anticoagulants and their role in preventing blood clots.
Key Takeaways
- Anticoagulants are drugs that prevent blood clot formation and are used to treat and prevent conditions like deep vein thrombosis, pulmonary embolism, and atrial fibrillation.
- They work by inhibiting clotting factors in the blood, with warfarin being a commonly used anticoagulant, and newer anticoagulants like DOACs offering similar efficacy with fewer drug interactions and no frequent blood monitoring.
- Bleeding is a common side effect of anticoagulant therapy, and the risk of bleeding is managed through regular blood coagulation level monitoring. Patients need to be educated on the signs of bleeding and when to seek medical attention.
- Anticoagulant therapy is crucial in preventing stroke and pulmonary embolism, and its effectiveness is measured through regular blood tests. Non-adherence to the medication increases the risk of clot formation, emphasizing the importance of medication adherence to patients.
The Importance of Anticoagulants in Preventing Blood Clots
The use of anticoagulants is crucial in preventing the formation of blood clots, as they effectively inhibit the coagulation process, ultimately reducing the risk of life-threatening events such as strokes and pulmonary embolisms.
One significant area where anticoagulants play a vital role is in surgery. During surgical procedures, the body’s natural response is to form blood clots to prevent excessive bleeding. However, these clots can sometimes obstruct blood flow, leading to serious complications. By administering anticoagulants, healthcare professionals can prevent the formation of these clots, ensuring that blood circulation remains unimpeded.
Another important application of anticoagulant therapy is in pregnancy. Pregnant women are at an increased risk of developing blood clots due to hormonal changes and reduced mobility. Anticoagulant therapy can help prevent clot formation, reducing the risk of complications such as deep vein thrombosis and pulmonary embolism during pregnancy.
In both surgical and pregnancy contexts, anticoagulants play a vital role in maintaining the health and well-being of individuals.
Mechanisms of Action: How Anticoagulants Work in the Body
One key mechanism by which anticoagulants function in the body involves inhibiting the activity of specific proteins involved in the blood clotting process. Different anticoagulant drugs employ various mechanisms of action to achieve this effect.
For instance, heparin and low molecular weight heparins inhibit clotting factors such as thrombin and factor Xa. Warfarin, on the other hand, interferes with the production of vitamin K-dependent clotting factors. Direct oral anticoagulants (DOACs) like dabigatran, rivaroxaban, apixaban, and edoxaban directly target specific clotting factors, preventing their activation.
These mechanisms ultimately disrupt the clotting cascade and prevent the formation of blood clots.
It is important to consider potential drug interactions when using anticoagulants. Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and antiplatelet agents, can increase the risk of bleeding when used concomitantly with anticoagulants. Additionally, some drugs may affect the metabolism or clearance of anticoagulants, potentially altering their effectiveness or increasing the risk of adverse effects.
Therefore, healthcare professionals must carefully evaluate the use of other medications alongside anticoagulants to ensure patient safety and optimize therapeutic outcomes.
Types of Anticoagulants and Their Specific Uses
Different anticoagulant medications have specific uses based on their mechanism of action and target proteins involved in the clotting process. Here are some types of anticoagulants and their specific uses:
- Warfarin: This oral anticoagulant has been widely used for decades and is effective in preventing blood clots in conditions such as atrial fibrillation and deep vein thrombosis.
- Heparin: Typically administered intravenously or subcutaneously, heparin is commonly used in hospitals to prevent blood clots during surgeries or to treat conditions like pulmonary embolism.
- Direct oral anticoagulants (DOACs): These newer anticoagulants, including rivaroxaban and apixaban, have shown comparable efficacy to warfarin with fewer bleeding complications. They are used for conditions like venous thromboembolism and prevention of stroke in atrial fibrillation.
- Anticoagulant alternatives: Ongoing research is exploring new anticoagulant options, such as factor Xa inhibitors, which have shown promise in preventing blood clots without the need for routine monitoring.
As new anticoagulant research continues to advance, these medications offer alternative options for patients in need of anticoagulation therapy.
Common Conditions and Disorders Treated with Anticoagulants
Common conditions and disorders that necessitate the use of anticoagulants include atrial fibrillation, deep vein thrombosis, pulmonary embolism, venous thromboembolism, and the prevention of stroke.
Anticoagulants are commonly used to manage these conditions and prevent the formation of blood clots.
Treatment options for atrial fibrillation typically involve the use of anticoagulant medication to reduce the risk of stroke.
Deep vein thrombosis and pulmonary embolism, which are caused by blood clots in the veins, are also treated with anticoagulants to prevent further clot formation and reduce the risk of complications.
Additionally, anticoagulants play a crucial role in the prevention and management of venous thromboembolism, a condition characterized by the formation of blood clots in the veins.
In summary, anticoagulants are essential in the treatment and prevention of various conditions and disorders, and medication management is crucial for optimizing patient outcomes.
Potential Side Effects and Risks of Anticoagulant Therapy
Adverse effects and potential risks are important considerations in the administration of anticoagulant therapy. Anticoagulants are commonly used to prevent and treat blood clots, but they can also have side effects that need to be carefully monitored.
One of the main concerns with anticoagulant therapy is the risk of bleeding. While anticoagulants help to prevent blood clots, they can also inhibit the clotting process, increasing the risk of bleeding. This can manifest as nosebleeds, bruising, or prolonged bleeding after an injury or surgery. In some cases, anticoagulants can lead to more serious bleeding events, such as gastrointestinal bleeding or intracranial hemorrhage.
Another potential side effect of anticoagulant therapy is the development of heparin-induced thrombocytopenia, a condition where the medication causes a decrease in platelet count, leading to an increased risk of clotting.
Overall, while anticoagulants are effective in preventing blood clots, healthcare providers must carefully weigh the benefits against the potential risks and carefully monitor patients for any adverse effects.
Monitoring and Managing Anticoagulant Therapy
Monitoring and managing anticoagulant therapy requires diligent oversight to ensure patient safety and optimize treatment efficacy. One key aspect of this process is managing dosages. Anticoagulant medications, such as warfarin or heparin, have a narrow therapeutic range, meaning that the dosage must be carefully tailored to each individual patient.
Regular monitoring of the patient’s blood clotting time, often measured using a test called the international normalized ratio (INR), is necessary to ensure that the dosage is within the desired range. Adjustments to the dosage can then be made as needed to maintain the desired anticoagulant effect while minimizing the risk of bleeding.
In addition to monitoring dosages, healthcare providers may also explore alternative therapies for anticoagulation. Newer anticoagulant medications, such as direct oral anticoagulants (DOACs), may offer certain advantages over traditional anticoagulants. DOACs have a more predictable anticoagulant effect, require less frequent monitoring, and have fewer interactions with other medications and diet.
However, they may not be suitable for all patients, and individual factors such as kidney function and bleeding risk must be considered when selecting the most appropriate anticoagulant therapy.
Regular monitoring and careful management of anticoagulant therapy are essential to ensure its safety and effectiveness for patients.
Future Developments and Advancements in Anticoagulant Treatment
Moving forward from the discussion on monitoring and managing anticoagulant therapy, it is crucial to explore the future developments and advancements in this field. Ongoing research endeavors aim to improve the efficacy and safety of anticoagulant treatment.
One area of focus is the development of novel anticoagulants that offer a more targeted approach with fewer side effects. Additionally, researchers are exploring alternative treatments that can complement or even replace traditional anticoagulants. These include the investigation of natural compounds with anticoagulant properties and the use of gene therapy to regulate coagulation factors.
Furthermore, advancements in technology, such as wearable devices and real-time monitoring systems, hold promise for enhancing the management of anticoagulant therapy. Overall, future research and innovation in this field offer hope for more personalized and effective anticoagulant treatments, ultimately improving patient outcomes.
Frequently Asked Questions
What are the different types of blood clots that can be treated with anticoagulants?
Anticoagulants are used to treat different types of blood clots, including deep vein thrombosis (DVT) and pulmonary embolism. They work by inhibiting the clotting factors in the blood, preventing the formation and growth of blood clots.
Are there any alternative treatments for preventing blood clots besides anticoagulant therapy?
Alternative treatments for preventing blood clots include antiplatelet therapy, mechanical devices like compression stockings, and lifestyle modifications such as regular exercise. The efficacy of these alternative therapies varies and should be discussed with a healthcare professional.
Can anticoagulants be used to treat other conditions besides blood clots?
Anticoagulants have shown potential for treating autoimmune diseases by reducing inflammation and preventing blood clot formation. Additionally, they are used for stroke prevention by inhibiting the formation of blood clots in the brain’s blood vessels.
How long does it typically take for anticoagulant therapy to start working and prevent blood clots?
The average time for anticoagulant therapy to start working and prevent blood clots varies depending on the specific drug and individual patient factors. Dosage adjustment may be necessary to achieve the desired therapeutic effect.
Are there any lifestyle changes or dietary restrictions required when taking anticoagulants?
Lifestyle changes and dietary restrictions may be necessary when taking anticoagulants. These measures aim to minimize the risk of bleeding or other complications. It is important to follow medical advice and maintain a balanced diet while on anticoagulant therapy.









