What is a c-sections – explained in simple words
Definition of c-section
A C-section, also known as a Cesarean section, is a type of surgery that doctors use to deliver a baby. Instead of the baby coming out through the mother’s vagina, the baby is taken out through a small cut that the doctor makes in the mother’s belly. This is usually done when it’s not safe for the baby to come out the regular way.
Why it is called C-section
C-section is short for “cesarean section.” It is called this because it is believed that Julius Caesar, the Roman emperor, was born this way. The word “cesarean” comes from the Latin word “caesus” which means “cut.” So, a C-section is named that way because it involves making a cut in the mother’s abdomen to deliver the baby.
What are the 3 types of C-section
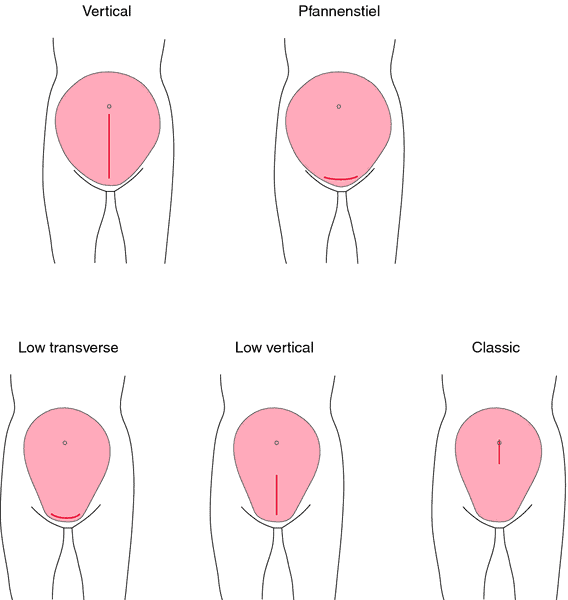
There are three main types of C-sections:
- Traditional C-section: Also known as a “vertical” or “classical” C-section, this is the most common type of C-section. It involves a large incision made across the mother’s abdomen and uterus.
- Low Transverse C-section: This type of C-section is also known as a “bikini cut” C-section. It involves a horizontal incision made low on the mother’s abdomen, just above the pubic hairline. This incision is usually smaller and allows for a faster recovery than a traditional C-section.
- Emergency C-section: An emergency C-section is performed when a vaginal delivery is not safe for the mother or the baby, and a C-section must be done immediately. This can happen due to unexpected complications during labor and delivery, such as placental abruption, fetal distress, or cord prolapse.
The choice of which type of C-section to perform depends on the situation and the condition of the mother and the baby and it should be discussed with a doctor or a gynecologist.
Reasons why a C-section may be necessary
Possible reasons why a C-section may be necessary may include:
- Fetal distress: If the baby is not getting enough oxygen during labor, a C-section may be necessary to deliver the baby quickly.
- Placental problems: If the placenta, which provides oxygen and nutrients to the baby, is not functioning properly, a C-section may be necessary to deliver the baby.
- Breech presentation: If the baby is not in the head-down position for delivery, a C-section may be necessary.
- Multiple pregnancies: If a woman is carrying more than one baby, a C-section may be necessary to deliver all of the babies safely.
- Previous C-section: If a woman has had a previous C-section, it may be recommended to have another C-section to avoid risks associated with vaginal delivery after cesarean.
- Health issues: If a woman has a health condition that makes vaginal delivery risky, such as hypertension, heart disease, or diabetes, a C-section may be necessary.
- Labor not progressing: If labor is not progressing as expected, despite the use of medical interventions to induce labour, a C-section may be necessary to avoid prolonging labor.
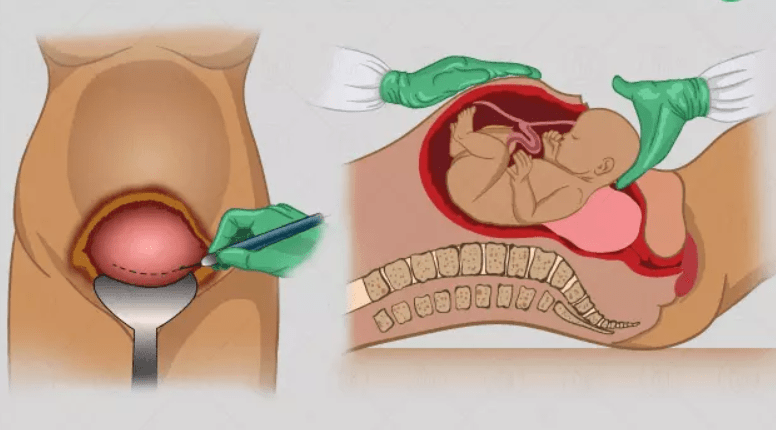
Description of what happens during c-section procedure
A C-section is a surgical procedure used to performed when a vaginal delivery is not safe for the mother or the baby.
During a C-section, the mother will be given anesthetic to numb the lower half of her body, so she won’t feel any pain during the procedure. The doctor will make a small cut in the mother’s abdomen and uterus, and then gently lift the baby out through the opening. The doctor will then close the incision with stitches or staples. The whole procedure takes about 30 to 60 minutes.
After the baby is born, the mother and baby will be closely monitored for any complications. The mother will be given medication to manage pain and will be moved to a recovery room for observation. The baby will also be checked by a pediatrician. The mother and baby will stay in the hospital for several days to recover.
Risks and benefits
Like any surgical procedure, C-sections come with both risks and benefits. It’s important to understand these risks and benefits when considering a C-section or when a C-section is recommended.
Benefits:
- C-sections are considered safe procedures, and in certain circumstances, they can save the lives of both the mother and the baby.
- C-sections may be necessary when vaginal delivery is not safe for the mother or the baby, such as in cases of fetal distress or placenta problems.
- C-sections allow for planned delivery, which can be beneficial for mothers with health conditions that make vaginal delivery risky.
- C-sections can also be beneficial for mothers carrying multiples, since it allows for the delivery of all babies at once.
Risks:
- C-sections are major surgeries, and like any surgery, there are risks associated with the procedure. These risks include infection, bleeding, blood clots, and injury to organs.
- C-sections also have a longer recovery time than vaginal delivery, and the mother may experience pain and discomfort around the incision site.
- C-sections may also increase the risk of complications during future pregnancies, such as placenta previa, placental abruption and uterine rupture.
- C-sections may also have an effect on the bonding between mother and baby, as recovery can be longer and the baby may be away from the mother for a short period of time.
Recovery process
Pain management
The mother will be given medication to manage any pain or discomfort around the incision site.
Incision care
The mother will be instructed on how to care for the incision, including how to keep the area clean and dry, and when to change dressings.
Rest and recovery
It’s important to rest as much as possible during the first few days after the surgery. The mother should avoid lifting heavy objects and strenuous activities, and should take it easy to allow the body to heal.
Follow-up appointments
The mother will have follow-up appointments with her doctor to check on her recovery and monitor the incision.
Monitoring the baby
The baby will be closely monitored by a pediatrician to ensure that they are healthy and well.
Breastfeeding
The mother will be given guidance on how to establish breastfeeding with her baby, if she chooses to do so.
Emotional support
It’s important to have emotional support during the recovery process, whether it’s from a partner, family member, or friend.
Physical therapy
Some mothers may need physical therapy to regain strength and mobility, especially if they have difficulty moving around.

Tips how to prepare mentally and emotionally
Preparing mentally and emotionally for a C-section can be challenging, but it’s important to be informed and to have a positive attitude towards the procedure. Here are some tips to help with the mental and emotional preparation:
- Learn about the procedure: Learn as much as you can about the C-section procedure, its risks, and benefits. This will help you make an informed decision and feel more in control of the situation.
- Talk to your doctor: Discuss your concerns and any questions you may have with your doctor. They will be able to provide you with accurate information and support.
- Have a support system: Surround yourself with people you trust and who can support you emotionally during the procedure and recovery.
- Be open-minded: Be open-minded about the delivery and understand that sometimes plans may change and unexpected things happen.
- Have realistic expectations: Understand that recovery after a C-section can take longer than a vaginal delivery and plan accordingly.
- Practice self-care: Take care of yourself both physically and emotionally. Try to relax, meditate, or practice yoga to help reduce stress.
- Seek counseling: If you feel overwhelmed, consider seeking counseling or therapy to help you cope with the emotional stress of the procedure.
- Remember that your baby’s safety comes first: The most important thing is the safety of you and your baby, so try to focus on that, and trust that your doctors medical specialists will do their best to deliver your baby safely.
It’s normal to have concerns and to feel emotional about a C-section. But with the right preparation and support, you can feel more in control of the situation and have a positive experience.
5 tips how to prepare physically
By being prepared physically, emotionally and mentally, you will feel more in control of the situation and better equipped to cope with the recovery process after a C-section. Try these 5 tips on how to prepare physically for c-sections:
- Get in shape: To make the recovery process after a C-section easier, it’s important to be in good physical shape. Try to maintain a healthy diet and exercise regularly before the surgery.
- Make a birth plan: Having a birth plan in place can help you feel more in control of the situation. Discuss your preferences with your gynecologist and make sure they are aware of your wishes.
- Pack a hospital bag: Pack a bag with everything you’ll need for the hospital stay, including comfortable clothes for yourself and the baby, toiletries, and any medications you’re currently taking.
- Arrange for help at home: Make sure you have someone who can help you at home during the recovery period. This can be a partner, family member, or friend.
- Practice breathing and relaxation techniques: Learn and practice breathing and relaxation techniques such as yoga, meditation, or progressive muscle relaxation. These can help you stay calm and focused during the procedure, and also aid in pain management.
Short-term complications
We already know that C-sections is generally a safe procedure, but like any surgery, there are short-term complications that can occur. Some of the most common short-term complications include:
- Infection: The incision site can become infected, which can cause redness, swelling, and pain. Antibiotics are usually prescribed to treat an infection.
- Bleeding: Some bleeding is normal after a C-section, but heavy bleeding can be a sign of a complication. Blood transfusions may be necessary in some cases.
- Blood clots: Blood clots can form in the legs or lungs after a C-section. These clots can be dangerous if they travel to the lungs or brain.
- Injury to organs: There is a small risk of injury to the bladder or bowel during a C-section.
- Anesthesia complications: There are also some risks associated with anesthesia, such as allergic reactions or breathing difficulties.
- Nausea and vomiting: Some mothers may experience nausea and vomiting after a C-section, which can be caused by the anesthesia or the pain medication.
- Pain: The mother may experience pain and discomfort around the incision site, but this can be managed with medication.
Long-term complications
Some of the most common long-term complications include:
- Chronic pain: Some mothers may experience chronic pain around the incision site, which can be caused by nerve damage or scar tissue.
- Adhesions: Scar tissue can form inside the body after a C-section, which can cause organs to stick together. This can cause pain or bowel obstruction.
- Placental problems: Women who have had a C-section may be at a higher risk of placental problems during future pregnancies, such as placenta previa or placental abruption.
- Uterine rupture: There is a small risk of uterine rupture during future pregnancies, which can be dangerous for both the mother and the baby.
- Hysterectomy: In some rare cases, a hysterectomy (removal of the uterus) may be required to stop bleeding or repair damage to the uterus after a c-section.
- Longer recovery time: Recovery after a c-section takes longer than vaginal delivery and the mother may have difficulty moving around for the first few days.
- Future pregnancies: Women who have had a C-section are more likely to have a C-section in future pregnancies, which can increase the risks associated with multiple cesareans.
F.A.Q.
How many C-sections can a woman have?
The number of C-sections a woman can safely have depends on several factors, including the woman’s overall health, the condition of her uterus, and the reason for the previous C-sections.
In general, the risk of complications increases with each subsequent C-section. The risk of complications such as placenta previa, placental abruption, and uterine rupture is higher for women who have had multiple C-sections.
However, the American College of Obstetricians and Gynecologists (ACOG) states that most women who have had one or two prior low-transverse C-sections can safely have a vaginal birth after cesarean (VBAC) with proper counseling and close monitoring.
Women who have had multiple C-sections to discuss their options with their doctor or gynecologist. They will take into account the woman’s personal health history, as well as the risks and benefits of each option, to help the woman make an informed decision about her next delivery.
A woman may choose to have multiple C-sections due to personal reasons or if vaginal delivery is not safe for her and her baby in future pregnancies.
How long does a C-section last?
Typically, a C-section will last between 30 and 90 minutes, although it can take longer in certain cases. The duration of a C-section can vary depending on the specific circumstances of the procedure.
Can I live normal life after C-section?
Yes, it is possible to live a normal life after a C-section, but it can take some time to recover fully. The recovery process after a C-section can take longer than recovery from a vaginal delivery, and it’s important for the mother to take care of herself both physically and emotionally during this time.
How many stitches are in a C-section?
The number of stitches used in a C-section varies depending on the individual case.
In a traditional C-section (also called “vertical” or “classical” C-section), the incision is made vertically across the abdomen and uterus, which may require more stitches to close the incision as it’s typically larger than the one in a low transverse c-section.
A low transverse C-section, also known as a “bikini cut” C-section, an incision is made horizontally low on the mother’s abdomen, just above the pubic hairline. This incision is usually smaller and can require fewer stitches to close.
The use of staples instead of stitches is also a common practice, which can speed up the recovery time and decrease the risk of infection.
How long after C-section can you walk?
Typically, most women are able to start walking around within the first 24 hours after a C-section. However, it’s important to start with short, slow walks and gradually increase the distance and time as you feel more comfortable. It’s recommended to move around as soon as possible after a C-section to prevent blood clots and other complications.
When can I take bath after C-section?
When you can take a bath after a C-section will depend on your individual recovery and the advice of your medical specialist. Typically, most women are able to take a bath within the first week after a C-section, but it’s best to check with your doctor for specific instructions.
It’s important to avoid submerging the incision site in water, such as taking a bath or swimming, until the incision is fully healed and the stitches or staples have been removed. This is to prevent infection and to promote proper healing.
Initially, it’s recommended to take sponge baths or showers instead of a bath. This will allow you to keep the incision site clean and dry, without submerging it in water. You can also ask your doctor when you can have a bath.
Avoid using bubble baths or bath oils as they can cause irritation or allergic reactions. It’s best to stick to plain water or mild, fragrance-free soap during this time.
What should I do the night before my C-section?
If you are scheduled for a C-section, it’s important to be prepared for the procedure to help reduce stress and anxiety. Here are some things you can do the night before your C-section to help you feel more at ease:
- Pack your bag: Make sure you have everything you need for you and your baby, such as comfortable clothes, personal hygiene items, and any medications you may need.
- Make arrangements for your other children: If you have other children, make sure arrangements are in place for them to be cared for during the time you will be in the hospital.
- Eat a light dinner: You will be instructed not to eat or drink anything after midnight before the procedure, so make sure to eat a light dinner.
- Get some rest: Try to get a good night’s sleep the night before your C-section, as it will help you feel more energized and better prepared for the procedure.
- Be mentally prepared: It’s normal to feel anxious or stressed, but try to stay positive and focus on the end goal, which is to bring a new life into this world.
- Communicate with your partner: Talk to your partner about your feelings and any concerns you may have. They can provide emotional support and help you feel more at ease.
- Follow your doctor’s instructions: Make sure you understand all the instructions given by your doctor regarding what you should do the night before your C-section and the day of the procedure.
Summary of key points
C-sections, also known as Cesarean sections, are surgical procedures used to deliver a baby. They are usually performed when a vaginal delivery is not safe for the mother or the baby.
Short-term complications of C-sections include infection, bleeding, blood clots, injury to organs, anesthesia complications, nausea and vomiting, and pain. These complications can be treated quickly and are not serious, but it is important to be aware of them and to seek medical attention if necessary.
Long-term complications of C-sections include chronic pain, adhesions, placental problems, uterine rupture, hysterectomy, longer recovery time, and future pregnancies. These risks can be higher compared to vaginal deliveries but it’s important to remember that C-sections are usually performed when vaginal delivery is not safe for the mother or the baby, and the benefits of a c-section outweigh the risks in these cases.








