What Is Hypertensive Nephropathy And How Is It Diagnosed?
Hypertensive nephropathy is a common renal disorder that arises as a result of prolonged and poorly controlled hypertension. It is characterized by structural and functional changes in the kidneys, leading to progressive renal damage and ultimately, renal failure. Accurate and timely diagnosis of hypertensive nephropathy is vital for effective management and prevention of complications.
The diagnosis of hypertensive nephropathy involves a combination of clinical evaluation, blood pressure measurements, urine tests, imaging studies, and in certain cases, renal biopsy. Blood pressure measurements are crucial for identifying hypertension, a key risk factor for the development of hypertensive nephropathy.
Urine tests, such as urinalysis and measurement of urinary albumin excretion, help assess renal function and detect kidney damage. Imaging studies, such as ultrasound or computed tomography scans, aid in visualizing structural abnormalities in the kidneys.
Renal biopsy, although invasive, may be necessary to confirm the diagnosis and determine the extent of renal injury.
By understanding the diagnostic approaches for hypertensive nephropathy, healthcare professionals can accurately identify and manage this condition, leading to improved patient outcomes.
Key Takeaways
- Hypertensive nephropathy is defined as kidney damage caused by high blood pressure.
- Diagnosis of hypertensive nephropathy involves assessing renal function through parameters such as serum creatinine, estimated glomerular filtration rate (eGFR), and proteinuria.
- Electrolyte imbalances play an important role in assessing the severity of the disease.
- Treatment options for hypertensive nephropathy include medications such as ACE inhibitors and ARBs, as well as lifestyle changes involving diet, weight management, and exercise.
Understanding Hypertensive Nephropathy
Hypertensive nephropathy, a condition characterized by progressive kidney damage due to long-standing high blood pressure, poses a significant challenge in diagnosing and managing patients with renal complications.
The primary focus of managing hypertensive nephropathy lies in blood pressure management and dietary restrictions. In order to control the progression of kidney damage, strict blood pressure control is crucial. This is achieved through the use of antihypertensive medications, such as angiotensin-converting enzyme inhibitors or angiotensin receptor blockers.
In addition to medication therapy, lifestyle modifications, including a low-salt diet, regular exercise, and weight management, are recommended to optimize blood pressure control. Dietary restrictions may also include reducing protein intake to alleviate the burden on the kidneys.
Management of hypertensive nephropathy requires a multidisciplinary approach, involving close monitoring of blood pressure levels and adherence to dietary recommendations to slow down the progression of kidney damage.
Blood Pressure Measurements
Blood pressure measurements are crucial in the evaluation of hypertensive nephropathy and play a pivotal role in the diagnosis and management of this renal condition. Hypertensive nephropathy is characterized by high blood pressure that leads to damage in the kidneys. Blood pressure management is essential in preventing and slowing down the progression of kidney damage.
Regular blood pressure monitoring helps healthcare professionals assess the effectiveness of treatment and make necessary adjustments to medication dosages. Additionally, blood pressure measurements can help identify individuals at risk for hypertensive nephropathy and guide early interventions to prevent kidney damage.
While blood pressure measurements are the primary diagnostic tool for hypertensive nephropathy, alternative diagnostic methods such as renal imaging and urine tests may be utilized to confirm the diagnosis and assess the extent of kidney damage.
Urine Tests
Urine tests are essential in evaluating kidney function and detecting abnormalities in patients with suspected hypertensive nephropathy. One of the most commonly used urine tests is urine analysis, which involves examining the physical, chemical, and microscopic characteristics of urine. This test can provide valuable information about kidney health, including the presence of red and white blood cells, bacteria, and crystals.
Another important aspect of urine analysis in the diagnosis of hypertensive nephropathy is the evaluation of proteinuria. Proteinuria, the presence of excess protein in the urine, is a hallmark of kidney damage and can indicate the severity of hypertensive nephropathy. Various methods are available to measure proteinuria, such as the urine protein-to-creatinine ratio and the 24-hour urine protein excretion test. These tests help clinicians diagnose and monitor the progression of hypertensive nephropathy, guiding appropriate management strategies.
Imaging Studies
This section will discuss the use of imaging studies such as ultrasound and CT scans in evaluating kidney damage.
Ultrasound is a non-invasive imaging technique that uses sound waves to create images of the kidneys, allowing for the detection of abnormalities such as kidney stones or cysts.
CT scans, on the other hand, provide detailed cross-sectional images of the kidneys and surrounding structures, enabling the assessment of kidney size, shape, and function.
Ultrasound and CT Scans
Ultrasound and CT scans are commonly used imaging techniques to aid in the diagnosis of hypertensive nephropathy.
Ultrasound is a non-invasive and cost-effective method that uses sound waves to create images of the kidneys. It is particularly useful for evaluating kidney size, detecting any structural abnormalities, and assessing blood flow to the kidneys. Although ultrasound has high accuracy in identifying renal artery stenosis, it may not provide detailed information on the extent of renal damage.
On the other hand, CT scans provide more detailed images of the kidneys and surrounding structures. They can help identify any signs of kidney damage, such as scarring or cysts. Additionally, CT scans can detect other conditions that may be contributing to the patient’s hypertension. However, CT scans involve exposure to ionizing radiation, which may limit their use in certain patient populations.
Evaluating Kidney Damage
Ultrasound and CT scans are commonly used imaging techniques to evaluate the structure and anatomy of the kidneys. However, when it comes to evaluating kidney damage, additional tests are required. These tests aim to assess kidney function and identify risk factors associated with hypertensive nephropathy.
One of the most important tests used for evaluating kidney function is the measurement of glomerular filtration rate (GFR). GFR provides an estimate of how well the kidneys are filtering waste products from the blood. Other tests, such as blood and urine tests, can also provide valuable information about kidney function and identify risk factors, including elevated blood pressure, proteinuria, and abnormal electrolyte levels.
By evaluating kidney function and identifying risk factors, healthcare professionals can diagnose hypertensive nephropathy and determine the appropriate management strategies to prevent further kidney damage. Early identification and intervention are crucial for preserving kidney function and improving patient outcomes.
Renal Biopsy
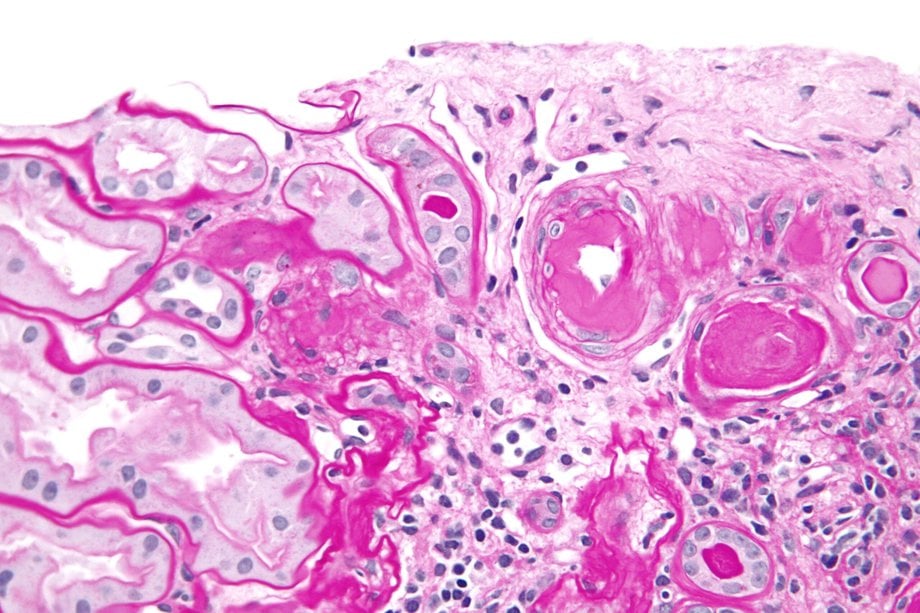
Renal biopsy is a diagnostic procedure used to confirm the diagnosis of hypertensive nephropathy.
It involves the removal of a small tissue sample from the kidney for microscopic examination.
The biopsy helps to assess the severity of the disease by evaluating the extent of damage to the renal structures, such as the glomeruli and tubules.
Confirming the Diagnosis
To establish the diagnosis of hypertensive nephropathy, various diagnostic methods can be employed. These methods aim to confirm the association between high blood pressure and kidney damage.
One of the primary diagnostic tools is blood pressure management. Consistently elevated blood pressure readings, especially in the absence of other causes, can suggest hypertensive nephropathy.
Additionally, alternative diagnostic methods can be utilized. Renal imaging techniques, such as ultrasound or magnetic resonance imaging (MRI), can help identify structural changes in the kidneys associated with hypertensive nephropathy.
Another alternative diagnostic method is the assessment of urinary protein levels. Increased proteinuria is commonly observed in patients with hypertensive nephropathy.
By employing these diagnostic methods, healthcare professionals can confirm the diagnosis of hypertensive nephropathy and initiate appropriate treatment strategies.
Assessing the Severity of the Disease
One way to evaluate the severity of hypertensive nephropathy is by assessing the extent of renal dysfunction and the presence of complications associated with the disease.
Assessing disease severity involves evaluating kidney damage, which can be done through various methods. One commonly used method is measuring the glomerular filtration rate (GFR), which provides an estimate of how well the kidneys are functioning. A decrease in GFR indicates a higher level of kidney damage and can help determine the severity of hypertensive nephropathy.
Additionally, assessing the presence of complications such as proteinuria, hypertension, and electrolyte imbalances can provide further insight into the severity of the disease.
These assessments help clinicians develop treatment plans and monitor the progression of hypertensive nephropathy to provide optimal care for patients.
Treatment Options
This section will discuss the treatment options for hypertensive nephropathy, focusing on two key points: medications to lower blood pressure and lifestyle changes to manage the disease.
Medications such as angiotensin-converting enzyme inhibitors (ACE inhibitors) and angiotensin receptor blockers (ARBs) are commonly prescribed to reduce blood pressure and protect the kidneys.
Additionally, lifestyle modifications such as maintaining a healthy weight, following a low-sodium diet, and regular exercise can also help manage hypertensive nephropathy.
Medications to Lower Blood Pressure
Several medications are available to lower blood pressure, offering a range of options for individuals with hypertensive nephropathy who aim to manage their condition effectively. These medications can help reduce blood pressure levels and slow the progression of kidney damage. Some commonly prescribed medications for hypertensive nephropathy include angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), diuretics, and calcium channel blockers.
It is important to note that the effectiveness of these medications can vary from person to person. Therefore, it may be necessary to try different medications or combinations of medications to find the most effective treatment plan. In some cases, alternative treatments such as lifestyle modifications, including a healthy diet low in salt and regular exercise, may also be recommended to help lower blood pressure and manage hypertensive nephropathy. It is crucial for individuals with this condition to work closely with their healthcare provider to determine the most suitable medication and treatment plan for their specific needs.
| Medication Type | Examples |
|---|---|
| ACE inhibitors | Lisinopril, Enalapril, Ramipril |
| Angiotensin Receptor Blockers | Losartan, Valsartan, Irbesartan |
| Diuretics | Hydrochlorothiazide, Furosemide, Spironolactone |
| Calcium Channel Blockers | Amlodipine, Nifedipine, Diltiazem |
Lifestyle Changes to Manage the Disease
Moving on from discussing medications to lower blood pressure, it is important to highlight the role of lifestyle changes in managing hypertensive nephropathy. Alongside medications, dietary modifications and an exercise regimen play a crucial role in controlling this condition.
Dietary modifications involve reducing sodium intake, limiting alcohol consumption, and increasing the consumption of fruits, vegetables, whole grains, and lean proteins. These changes can help lower blood pressure and reduce the strain on the kidneys.
Additionally, regular physical activity is recommended to improve cardiovascular health and maintain a healthy weight. Engaging in aerobic exercises, such as brisk walking or swimming, for at least 150 minutes per week is beneficial.
These lifestyle changes, when combined with medication, can effectively manage hypertensive nephropathy and improve overall kidney function.
Managing Complications
To effectively manage the complications associated with hypertensive nephropathy, it is imperative to implement a comprehensive treatment approach that addresses the underlying cause of the condition and focuses on blood pressure control, renal function preservation, and prevention of further kidney damage. Managing complications involves a combination of lifestyle modifications and medical interventions. Treatment options may include medications to control blood pressure, such as angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Additionally, diuretics may be prescribed to reduce fluid retention and lower blood pressure. In cases where kidney function is severely compromised, dialysis or kidney transplantation may be necessary. Regular monitoring of kidney function and blood pressure is essential to assess the effectiveness of treatment and make adjustments as needed. By actively managing complications, individuals with hypertensive nephropathy can slow the progression of kidney damage and improve their overall quality of life.
| Treatment Options | Benefits |
|---|---|
| Medications | Control blood pressure |
| Diuretics | Reduce fluid retention and lower blood pressure |
| Dialysis/Transplantation | Treat severe kidney dysfunction |
Long-Term Outlook and Prognosis
This paragraph will discuss two key points related to the long-term outlook and prognosis of hypertensive nephropathy: monitoring kidney function and preventing disease progression.
Monitoring kidney function is crucial in managing hypertensive nephropathy, as it allows healthcare professionals to assess the progression of the disease and make necessary interventions.
Additionally, preventing disease progression is essential in improving the long-term outlook of individuals with hypertensive nephropathy, and this can be achieved through lifestyle modifications, blood pressure control, and medication adherence.
Monitoring Kidney Function
One way to assess the renal function in patients with hypertensive nephropathy is through regular monitoring of kidney function parameters.
Monitoring kidney function is crucial to evaluate the progression of the disease and to guide appropriate management strategies.
Renal function assessment involves measuring various parameters, such as serum creatinine, estimated glomerular filtration rate (eGFR), and proteinuria.
Serum creatinine levels are commonly used to estimate kidney function, with higher levels indicating decreased renal function.
eGFR provides a more accurate estimation of kidney function by taking into account factors such as age, sex, and race.
Proteinuria, the presence of excess protein in the urine, is an important marker of kidney damage.
Regular monitoring of these parameters allows healthcare providers to detect any decline in renal function and adjust treatment accordingly, thereby optimizing patient outcomes.
Preventing Disease Progression
Preventing disease progression in patients with hypertensive nephropathy involves implementing strategies aimed at slowing the decline of kidney function and reducing the risk of complications. Disease prevention is crucial in managing hypertensive nephropathy, and lifestyle modifications play a significant role in achieving this goal.
Here are some key strategies that can help prevent disease progression:
- Blood pressure control: Maintaining optimal blood pressure levels is essential in slowing the progression of hypertensive nephropathy. This can be achieved through medication adherence, regular monitoring, and making necessary lifestyle changes.
- Dietary modifications: A healthy diet low in sodium and rich in fruits, vegetables, and whole grains can help reduce blood pressure and minimize kidney damage.
- Weight management: Achieving and maintaining a healthy weight can significantly improve kidney function and reduce the risk of complications.
- Regular exercise: Engaging in regular physical activity can help lower blood pressure, improve cardiovascular health, and positively impact kidney function.
- Smoking cessation: Smoking can worsen kidney damage and increase the risk of complications. Quitting smoking is crucial in preventing disease progression.
By implementing these strategies and making necessary lifestyle modifications, patients with hypertensive nephropathy can reduce the risk of complications and slow the decline of kidney function.
Frequently Asked Questions
What are the risk factors for developing hypertensive nephropathy?
The risk factors for developing hypertensive nephropathy include uncontrolled hypertension, long-term high blood pressure, age, obesity, family history, smoking, and certain medical conditions. Prevention methods include lifestyle modifications, such as maintaining a healthy weight and blood pressure, regular exercise, and avoiding smoking. Treatment options include medication to control blood pressure and manage kidney function.
Can hypertensive nephropathy be prevented?
Preventive measures for hypertensive nephropathy include maintaining a healthy blood pressure, following a balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption. Treatment options may include medication to control blood pressure and managing underlying conditions.
How does hypertensive nephropathy differ from other types of kidney disease?
Hypertensive nephropathy is a type of kidney disease that occurs as a result of long-term high blood pressure. It differs from other types of kidney disease in terms of its specific treatments and complications, such as medication management and the risk of kidney failure.
Are there any lifestyle changes that can help manage hypertensive nephropathy?
Diet modifications and exercise routines can help manage hypertensive nephropathy. These lifestyle changes can include reducing sodium intake, maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet rich in fruits and vegetables.
Is hypertensive nephropathy a reversible condition?
Hypertensive nephropathy is a potentially reversible condition. Treatment options for hypertensive nephropathy include controlling blood pressure, managing underlying conditions, and adopting a healthy lifestyle. However, the extent of reversibility may vary depending on the severity and duration of the disease.









