What is insulin resistance
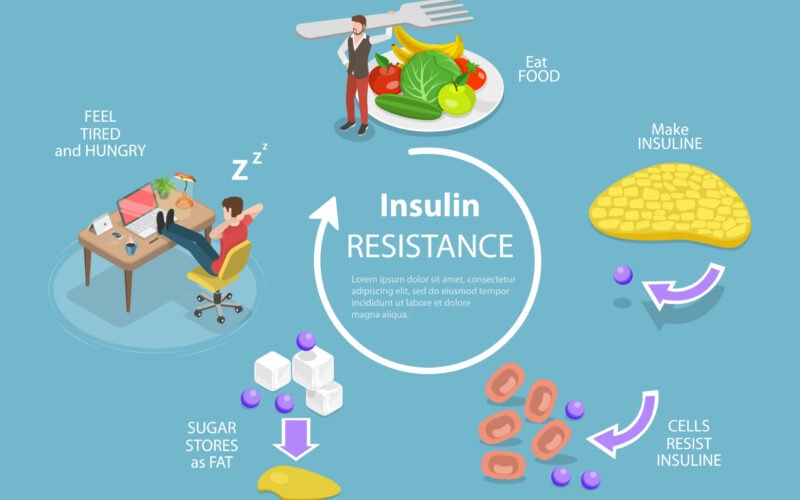
Insulin resistance is a condition in which the body’s cells do not respond properly to insulin, the hormone that regulates blood sugar levels. Insulin is a hormone produced by the pancreas that helps to regulate the amount of glucose (sugar) in the blood. When the body is resistant to the effects of insulin, it needs more insulin than normal to keep blood sugar levels in the normal range.
How insulin resistance develops
Insulin resistance can occur when the body’s cells don’t respond normally to insulin, making it difficult for glucose to enter the cells and be used for energy. This can cause the pancreas to produce more insulin to try to get the glucose into the cells, leading to higher than normal insulin levels in the blood.
Factors contributing to the development of insulin resistance:
- Being overweight or obese
- Lack of physical activity
- High blood pressure
- High cholesterol
- A diet high in processed foods and sugar
- Genetics, certain genetic variants are associated with insulin resistance
- Polycystic ovary syndrome (PCOS) or acanthosis nigricans
- Glucocorticoids, atypical antipsychotics.
If insulin resistance persists over time, it can lead to prediabetes and type 2 diabetes. Insulin resistance can also increase the risk of other health problems such as heart disease, stroke and nonalcoholic fatty liver disease.
How insulin resistance is diagnosed
Insulin resistance is typically diagnosed through a combination of clinical signs and symptoms, laboratory tests, and other diagnostic tools. The most common ways to diagnose insulin resistance include:
- Fasting glucose and insulin test: A blood test that measures glucose and insulin levels in the blood after an overnight fast. Elevated insulin levels in the presence of normal or only slightly elevated glucose levels can indicate insulin resistance.
- Oral glucose tolerance test (OGTT): A blood test that measures glucose and insulin levels after a person has consumed a sugary drink. An abnormal OGTT can indicate insulin resistance, prediabetes, or diabetes.
- HbA1c: This test measures the average blood sugar level over the past 2-3 months. A HbA1c level of 5.7-6.4% is considered prediabetes, and a level of 6.5% or higher indicates diabetes.
- Homeostatic model assessment (HOMA-IR) : This is a mathematical calculation that estimates the level of insulin resistance in the body based on fasting glucose and insulin levels. A high HOMA-IR score indicates insulin resistance.
- Euglycemic hyperinsulinemic clamp: This is considered the gold standard test for assessing insulin resistance, but it is an invasive test that requires an IV line and it’s not widely used in clinical practice.
Who can diagnose insulin resistance
Insulin resistance can be diagnosed by a variety of medical specialist, including:
- Primary care physicians – General practitioners, family physicians, and internists are often the first medical specialist to diagnose insulin resistance. They can perform initial evaluations, order laboratory tests and refer to specialists if needed.
- Endocrinologists – Endocrinologists are specialists in hormones and metabolism. They can evaluate and diagnose insulin resistance, as well as manage and treat patients with diabetes and other endocrine disorders.
- Diabetologists – These are specialists in diabetes and its complications, they can diagnose and manage diabetes and its related metabolic disorders such as insulin resistance.
- Dietitians and nutritionists – They can provide guidance on healthy eating and lifestyle changes that can help manage insulin resistance and prevent the progression to diabetes.
- Nurse practitioners and physician assistants – They can also evaluate and diagnose insulin resistance, order laboratory tests and refer to specialists if needed.
What to do if insulin resistance is diagnosed
If you are diagnosed with insulin resistance, there are several steps you can take to manage the condition and reduce your risk for developing diabetes and other health problems:
- Lifestyle changes – Making healthy lifestyle changes can help improve insulin sensitivity and reduce the risk of developing diabetes. This includes regular physical activity, eating a healthy diet that is low in processed foods and sugar, and maintaining a healthy weight.
- Diet – Eating a diet that is rich in whole foods, lean protein, healthy fats, and non-starchy vegetables can help lower blood sugar levels and improve insulin sensitivity. Avoiding processed foods and added sugars, and limiting the intake of refined carbohydrates can also be beneficial.
- Exercise – Regular physical activity is one of the most effective ways to improve insulin sensitivity. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Medications – Metformin, a medication commonly used to treat type 2 diabetes, can help improve insulin sensitivity. Your doctor may also prescribe other medications to help lower blood sugar levels and improve insulin sensitivity.
- Monitoring – Regular monitoring of blood sugar levels and HbA1c test is important to track the progress of the treatment and to adjust it if needed.
- Follow-up – Keep in touch with your doctor, and attend your follow-up appointments to make sure you are on track and to make any necessary adjustments to your treatment plan.
Treatments for insulin resistance
There are several treatment options available for insulin resistance, including:
Lifestyle changes
Making healthy lifestyle changes is the first line of treatment for insulin resistance. This includes regular physical activity, eating a healthy diet that is low in processed foods and sugar, and maintaining a healthy weight.
Diet
Eating a diet that is rich in whole foods, lean protein, healthy fats, and non-starchy vegetables can help lower blood sugar levels and improve insulin sensitivity. Avoiding processed foods and added sugars, and limiting the intake of refined carbohydrates can also be beneficial.
Exercise
Regular physical activity is one of the most effective ways to improve insulin sensitivity. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Medications
Metformin, a medication commonly used to treat type 2 diabetes, can help improve insulin sensitivity. Other medications such as thiazolidinediones, GLP-1 receptor agonists and DPP-4 inhibitors can also be used to improve insulin sensitivity.
Bariatric surgery
In some cases, particularly in individuals with severe obesity and insulin resistance, bariatric surgery (weight loss surgery) may be considered as a treatment option.
Herbal supplements
Some supplements such as berberine, omega-3 fatty acids, and cinnamon can also help improve insulin sensitivity. However, it’s important to note that these supplements should be used under the guidance of a medical specialist, as they may interact with other medications or have side effects.
Recommendations
Early detection and management of insulin resistance can prevent or delay the progression to type 2 diabetes. Your doctor can perform a glucose tolerance test, a hemoglobin A1c test and other tests to determine if you have insulin resistance and work with you to establish a plan to manage your risk for developing type 2 diabetes by making lifestyle changes such as eating a healthy diet, exercising regularly, and maintaining a healthy weight.







