What Is the Connection Between Retinal Detachment and Trauma
Retinal detachment is a serious ocular condition that can result in permanent vision loss if not promptly treated.
Trauma has been identified as one of the potential causes of retinal detachment, but the specific connection between the two remains unclear.
This article aims to explore the relationship between retinal detachment and trauma by examining the underlying causes, understanding the anatomy of the retina, recognizing the signs and symptoms, discussing diagnostic tests, exploring treatment options, and evaluating the recovery and prognosis associated with traumatic retinal detachment.
Key Takeaways
- Retinal detachment can be caused by direct trauma to the eye, such as blunt force or penetrating injury, as well as indirect trauma from rapid acceleration or deceleration forces.
- The severity and location of the trauma determine the likelihood and extent of retinal detachment.
- Sharp objects or projectiles can cause tears or holes in the retina, leading to detachment.
- Pre-existing eye conditions and age-related changes can also increase the risk of retinal detachment following trauma.
Causes of Retinal Detachment Related to Trauma
Causes of retinal detachment related to trauma include direct trauma to the eye, such as a blunt force or penetrating injury, as well as indirect trauma, such as rapid acceleration or deceleration forces on the head and eye.
The impact of trauma on the retina can result in the separation of the retina from the underlying tissue layers, leading to retinal detachment. Direct trauma, such as a sharp object penetrating the eye, can cause a tear or hole in the retina, allowing fluid to accumulate between the layers and detach the retina.
Indirect trauma, such as a sudden acceleration or deceleration force, can create shearing forces within the eye, also leading to retinal detachment. The severity of the trauma and the location of the impact can determine the likelihood and extent of retinal detachment.
Therefore, understanding the causes of retinal detachment related to trauma is crucial for prompt diagnosis and treatment.
Understanding the Anatomy of the Retina
The understanding of the anatomy of the retina is essential in comprehending the underlying mechanisms involved in the occurrence of retinal detachment following trauma. The retina is a complex structure consisting of several layers, each with specific functions in vision. The outermost layer, the retinal pigment epithelium (RPE), provides nourishment and support to the underlying layers. The photoreceptor layer, which includes rods and cones, is responsible for converting light into electrical signals. The innermost layer, the ganglion cell layer, contains the cell bodies of the retinal ganglion cells, which transmit visual information to the brain via the optic nerve. Disruption or damage to any of these layers can lead to retinal detachment.
Table: Risk factors for retinal detachment following trauma
| Risk Factors | Examples |
|---|---|
| High-impact trauma | Motor vehicle accidents, falls from height |
| Penetrating trauma | Sharp objects, projectiles |
| Pre-existing eye conditions | Myopia, previous retinal detachment |
| Age-related changes | Vitreous liquefaction, posterior vitreous detachment |
Understanding the anatomy of the retina is crucial in developing strategies for retinal detachment prevention and identifying individuals at risk for this condition. By recognizing the risk factors associated with trauma, healthcare professionals can take appropriate measures to prevent retinal detachment and provide timely treatment if necessary.
Signs and Symptoms of Retinal Detachment From Trauma
The occurrence of trauma-induced retinal detachment can lead to significant visual changes in individuals. Recognizing these visual changes is crucial in order to identify and diagnose retinal detachment in a timely manner.
Understanding the signs and symptoms associated with trauma-induced retinal detachment is important for healthcare professionals and individuals alike, as early detection and treatment can help prevent permanent vision loss.
Trauma-Induced Retinal Detachment
Trauma-induced retinal detachment occurs as a result of physical injury to the eye. The causes of trauma-induced retinal detachment can vary, but common factors include direct trauma to the eye, such as blunt force or penetrating injuries, and indirect trauma, such as rapid acceleration or deceleration forces. Other causes may include sports-related injuries, motor vehicle accidents, falls, or assault. To prevent traumatic retinal detachment, several strategies can be employed. These include wearing appropriate protective eyewear during activities that pose a risk of eye injury, such as contact sports or construction work. Additionally, promoting awareness about eye safety and encouraging early treatment for eye injuries can help minimize the risk of trauma-induced retinal detachment.
| Causes of Trauma-Induced Retinal Detachment | Prevention Strategies for Traumatic Retinal Detachment |
|---|---|
| Direct trauma to the eye | Wearing protective eyewear during high-risk activities |
| Indirect trauma (acceleration or deceleration) | Promoting awareness about eye safety |
| Sports-related injuries | Encouraging early treatment for eye injuries |
| Motor vehicle accidents | |
| Falls | |
| Assault |
Recognizing Visual Changes
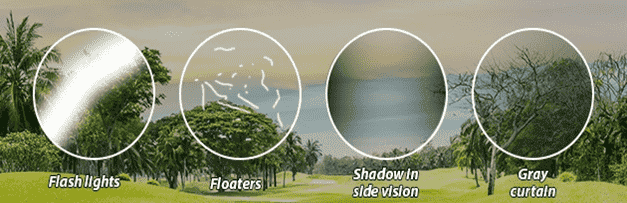
Visual changes can serve as a key indicator for the presence of trauma-induced retinal detachment. In cases of retinal detachment caused by trauma, individuals may experience a range of visual symptoms that can significantly impact their daily life. These symptoms can include sudden flashes of light, a sudden increase in floaters, a curtain-like shadow appearing in the peripheral vision, or a decrease in visual acuity.
Detecting these changes in visual perception is crucial for early diagnosis and prompt treatment, as untreated retinal detachment can lead to permanent vision loss. The impact on daily life can be substantial, as visual changes may affect an individual’s ability to perform tasks requiring good vision, such as reading, driving, or recognizing faces. Therefore, prompt recognition and intervention are essential to preserve visual function and minimize the impact on daily activities.
Diagnostic Tests for Traumatic Retinal Detachment
The accuracy of diagnostic tests for traumatic retinal detachment plays a crucial role in identifying and confirming this condition.
Various imaging techniques are used to aid in the accurate diagnosis of retinal detachment, such as ultrasound, optical coherence tomography (OCT), and fundus photography.
These imaging techniques provide valuable information about the location, extent, and severity of retinal detachment, allowing for appropriate treatment decisions to be made.
Accuracy of Diagnostic Tests
Based on the available literature, the accuracy of diagnostic tests for retinal detachment in relation to trauma is a topic of ongoing investigation. The accurate diagnosis of retinal detachment is crucial for timely intervention and prevention of permanent vision loss.
Various imaging techniques have been used to aid in the diagnosis of this condition, including ultrasound, optical coherence tomography (OCT), and fundus photography. Ultrasound is considered a reliable method for identifying retinal detachment and determining its extent.
OCT provides high-resolution cross-sectional images of the retina, which can aid in the visualization and characterization of retinal detachment. Fundus photography can also be helpful in detecting retinal breaks and identifying the extent of detachment.
However, the accuracy of these imaging techniques in diagnosing retinal detachment in trauma cases is still being investigated, and further research is needed to establish their reliability and effectiveness in this specific context.
Role of Imaging Techniques
Ultrasound, optical coherence tomography (OCT), and fundus photography are imaging techniques commonly employed for the diagnosis of retinal detachment. These advanced technologies play a crucial role in accurately identifying and characterizing retinal detachment, aiding in guiding appropriate treatment decisions.
The future developments in imaging techniques hold promise for further improving the diagnosis and management of retinal detachment. Some potential advancements include:
- Enhanced resolution: Advancements in imaging technology may lead to higher resolution images, allowing for better visualization of the retinal layers and finer details of the detachment.
- Real-time imaging: The development of real-time imaging techniques would provide clinicians with immediate feedback during procedures, assisting in precise and efficient treatment delivery.
- Automated analysis: Future developments may include the implementation of artificial intelligence algorithms, enabling automated analysis of retinal images and assisting in accurate diagnosis.
- Non-invasive imaging: Non-invasive imaging techniques hold potential for minimizing patient discomfort and reducing the risk of complications associated with invasive procedures.
These future advancements in imaging technology are expected to revolutionize the diagnosis and management of retinal detachment, improving patient outcomes and ensuring timely interventions.
Treatment Options for Retinal Detachment Caused by Trauma
Surgical intervention is often recommended for the treatment of retinal detachment caused by trauma. The goal of treatment is to reattach the retina and restore normal vision.
Various treatment options are available, including pneumatic retinopexy, scleral buckling, and vitrectomy. Pneumatic retinopexy involves injecting a gas bubble into the eye to push the detached retina back into place. Scleral buckling involves placing a silicone band around the eye to provide support and push the detached retina back into position. Vitrectomy is a surgical procedure where the vitreous gel inside the eye is removed and replaced with a gas or silicone oil to reattach the retina.
The choice of treatment depends on factors such as the location and extent of detachment, the patient’s age, and the surgeon’s preference. The recovery prognosis varies depending on the severity of the detachment and the success of the surgical intervention. Regular follow-up visits are essential to monitor the progress and ensure proper healing.
Recovery and Prognosis for Traumatic Retinal Detachment
The recovery and prognosis for traumatic retinal detachment can vary depending on factors such as the severity of the detachment and the success of the chosen treatment method. While some individuals may experience full recovery and restoration of vision, others may have long-term complications or partial vision loss.
The prognosis for traumatic retinal detachment is influenced by various factors, including:
- Severity of the detachment: The extent and location of the detachment can affect the chances of successful recovery.
- Promptness of treatment: Early intervention can improve the chances of successful reattachment and better visual outcomes.
- Underlying causes: Trauma can result from various causes, such as accidents or eye injuries. The specific cause may impact the prognosis.
- Overall eye health: The condition of the eye prior to the detachment can influence the recovery process.
Understanding these factors can help healthcare professionals provide appropriate treatment and manage expectations for individuals with traumatic retinal detachment.
Frequently Asked Questions
Can Retinal Detachment Occur Without Any Trauma or Injury?
Retinal detachment can occur without trauma or injury; however, trauma is a known risk factor. Other causes include aging, myopia, and previous eye surgery. Treatment options for retinal detachment include surgery, such as scleral buckling or vitrectomy.
Are There Any Specific Risk Factors That Increase the Likelihood of Retinal Detachment From Trauma?
The likelihood of retinal detachment from trauma is influenced by specific risk factors. Understanding these risk factors is important in identifying individuals who may be more prone to experiencing retinal detachment following a traumatic event.
What Are the Different Types of Traumatic Retinal Detachment and How Do They Differ in Terms of Severity and Treatment?
The different types of traumatic retinal detachment can be classified based on severity. Surgical options are available for treatment. Severity classification and surgical options are important considerations when managing traumatic retinal detachment.
Is It Possible for a Person to Experience Symptoms of Retinal Detachment From Trauma Immediately After the Injury or Can It Take Some Time for the Symptoms to Manifest?
The manifestation of symptoms of retinal detachment after trauma can vary. In some cases, immediate symptoms may be present, while in others, symptoms may take some time to manifest.
Are There Any Preventive Measures That Can Be Taken to Reduce the Risk of Retinal Detachment From Trauma?
Preventive measures for retinal detachment from trauma can reduce the risk factors associated with this condition. These measures aim to minimize the likelihood of traumatic injury to the eye and include the use of protective eyewear and adherence to safety guidelines.








