Blood Types And Compatibility: Crucial Factors In Transplants
Blood transfusions and organ transplants are life-saving medical procedures that have become increasingly common in modern medicine. However, the success of these procedures depends heavily on the compatibility of blood types between the donor and recipient.
Blood typing and compatibility testing are crucial factors in ensuring that the patient receives a safe and effective transplant. The human blood system is complex and diverse, with many different blood types and antigens that can trigger immune responses.
Understanding the basics of blood typing and compatibility is essential for healthcare professionals in the field of transplantation. In this article, we will explore the four blood types, the importance of the Rh factor, and how cross-matching and testing for rejection play a critical role in determining blood compatibility.
We will also discuss the risks and complications of incompatible transplants and the advances in transplant technology that are improving outcomes for patients.
Key Takeaways
- Compatibility of blood types between donor and recipient is crucial for successful transplant procedures.
- Incompatible transplants can lead to adverse reactions, complications, and even death.
- Universal donors have type O negative blood, while universal recipients have type AB positive blood.
- Bioengineering and regenerative medicine offer potential solutions to the shortage of donor organs and can reduce the risk of rejection.
The Basics of Blood Typing and Antigens
The identification of blood types and antigens is a fundamental component in the understanding of blood compatibility and is essential in facilitating successful organ transplants.
Blood types are determined by the presence or absence of specific antigens on the surface of red blood cells. There are four main blood types: A, B, AB, and O. Type A blood has A antigens on the surface of the red blood cells, type B has B antigens, type AB has both A and B antigens, and type O has neither A nor B antigens. Additionally, each blood type can be either positive or negative, depending on the presence or absence of the Rh factor antigen.
Antigens play a critical role in blood compatibility because they can trigger an immune response from the body. For example, if a person with type A blood receives a transfusion of type B blood, the A antigens on the surface of the red blood cells will be recognized as foreign by the recipient’s immune system, and an immune response will be triggered. This can lead to a range of complications, including fever, chills, and potentially life-threatening reactions.
Therefore, it is essential to match the blood type and Rh factor of the donor and recipient in order to minimize the risk of adverse reactions and optimize the success of organ transplants.
Understanding the Four Blood Types
Understanding the different antigens present on the surface of red blood cells is key to comprehending blood group classification. The four main blood types are A, B, AB, and O, which are determined by the presence or absence of certain antigens.
To further clarify, here are three sub-lists that distinguish each blood type:
- Type A blood has the A antigen on the surface of the red blood cells and produces anti-B antibodies in response to the B antigen.
- Type B blood has the B antigen on the surface of the red blood cells and produces anti-A antibodies in response to the A antigen.
- Type AB blood has both A and B antigens on the surface of the red blood cells and does not produce any antibodies against either A or B antigens.
Knowing the different blood types is essential in transfusion and transplantation procedures as certain blood types are incompatible with others. For example, if a person with type A blood receives a transfusion of type B blood, their immune system will recognize the foreign B antigen and produce antibodies against it, resulting in an adverse reaction.
Therefore, a thorough understanding of blood types and compatibility is crucial in medical procedures to ensure the safety and well-being of patients.
The Importance of the Rh Factor
An essential consideration in medical procedures involving blood transfusions and pregnancies is the presence or absence of the Rh factor on the surface of red blood cells. The Rh factor is a protein that can be either present (+) or absent (-) on the surface of red blood cells. If a person has the Rh factor, they are Rh positive (+), and if they do not have it, they are Rh negative (-). This factor is crucial in blood transfusions because if a person with Rh-negative blood receives Rh-positive blood, their immune system may attack the foreign blood cells, causing a reaction that can be life-threatening.
The presence or absence of the Rh factor is also important in pregnancies. If a woman with Rh-negative blood is carrying a fetus with Rh-positive blood, there is a risk of hemolytic disease of the newborn (HDN). This occurs when the mother’s immune system produces antibodies against the Rh factor in the fetus’s blood, which can lead to anemia, jaundice, brain damage, and even death. To prevent HDN, Rh-negative women are given an injection of Rh immunoglobulin during pregnancy and after delivery if the baby is Rh positive. Overall, understanding the Rh factor is essential in medical procedures involving blood transfusions and pregnancies to ensure compatibility and prevent adverse reactions.
| Blood Type | Rh Factor | Can Receive from | Can Donate to |
|---|---|---|---|
| A | + | A+, AB+ | A+, O+ |
| A | – | A+, A-, AB+, AB- | A+, AB+ |
| B | + | B+, AB+ | B+, O+ |
| B | – | B+, B-, AB+, AB- | B+, AB+ |
| AB | + | AB+ | A+, B+, AB+, O+ |
| AB | – | AB+, AB-, A+, A-, B+, B-, O+, O- | AB+, AB- |
| O | + | A+, B+, AB+, O+ | O+ |
| O | – | A+, A-, B+, B-, AB+, AB-, O+, O- | O+, O- |
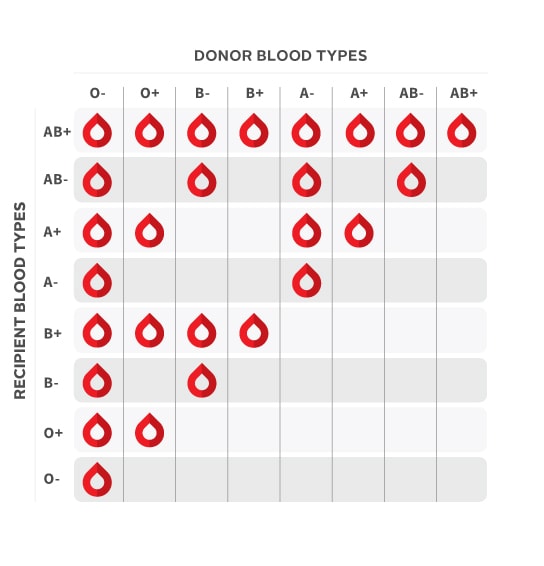
Determining Blood Compatibility
Determining the suitability of blood for transfusions and pregnancies requires a thorough analysis of the Rh factor and other pertinent factors.
Blood type compatibility depends on the presence or absence of specific antigens on the surface of red blood cells and antibodies in the plasma.
ABO and Rh are the most important blood group systems, but there are over 30 other blood group systems that can also influence transfusion reactions.
To determine blood compatibility, the donor’s blood type must be tested against the recipient’s blood type.
If the donor’s blood type contains antigens that the recipient’s blood type lacks, the recipient’s immune system may attack and destroy the donor’s red blood cells, leading to a transfusion reaction.
In general, individuals with type O negative blood are considered universal donors because their blood lacks A, B, and Rh antigens, while individuals with type AB positive blood are considered universal recipients because their blood contains all A, B, and Rh antigens.
However, even with a perfect match, other factors such as antibodies, white blood cells, and platelets can still cause reactions.
Therefore, careful testing and analysis is necessary to minimize the risk of complications and ensure successful transfusions and pregnancies.
Cross-Matching and Testing for Rejection
Cross-matching and testing for rejection is a critical step in ensuring the success of transfusions and pregnancies. In cross-matching, the recipient’s serum is mixed with the donor’s red blood cells to check for compatibility. Compatibility is determined by the absence of agglutination or clumping of the red blood cells. This test is necessary to prevent hemolytic transfusion reactions, which can lead to severe complications such as kidney failure, shock, and death.
Testing for rejection is also vital in ensuring the success of transplants. The immune system can recognize foreign tissues and attack them, leading to rejection. Various tests such as tissue typing, cross-matching, and panel-reactive antibody testing are conducted to determine the likelihood of rejection. In cases where the recipient has high levels of antibodies against the donor’s tissue, desensitization therapy may be needed to reduce the antibody levels and increase the likelihood of a successful transplant. Through cross-matching and testing for rejection, medical professionals can ensure that transfusions and transplants are successful, saving countless lives.
| Blood Type | Can Donate to | Can Receive from | Compatibility |
|---|---|---|---|
| O- | Anyone | O- | Universal |
| A- | A-, AB- | A-, O- | Limited |
| B- | B-, AB- | B-, O- | Limited |
| AB- | AB- | Everyone | Universal |
| Rh+ | Rh+ | Rh+, Rh- | Common |
The table above demonstrates the compatibility of different blood types. While some blood types can donate to and receive from anyone, others have limited compatibility. The table also highlights the importance of the Rh factor in determining compatibility. Individuals with Rh+ blood can receive from both Rh+ and Rh- donors, while those with Rh- blood can only receive from Rh- donors. The table can evoke an emotional response in the audience by emphasizing the importance of knowing one’s blood type and the impact it can have on receiving life-saving treatments.
Finding a Suitable Donor
Identifying a suitable donor is a critical step in ensuring the success of medical procedures that involve transferring biological material from one individual to another. In the case of blood transfusions or organ transplants, finding a compatible donor is essential to avoid rejection by the recipient’s immune system.
There are several factors to consider when searching for a donor, such as blood type, tissue type, and genetic compatibility.
To find a suitable donor for a blood transfusion, the medical staff must determine the recipient’s blood type and find a donor with the same blood type. This is because the immune system recognizes foreign antigens on the surface of red blood cells, and if the recipient receives blood with an antigen they do not possess, their immune system will attack the transfused blood cells.
For organ transplants, the medical team must consider not only the blood type but also the tissue type and genetic compatibility between the donor and recipient. The closer the match, the less likely the recipient’s immune system will reject the transplanted organ.
Finding a compatible donor can be a challenging task, requiring extensive testing and careful consideration of multiple factors.
Risks and Complications of Incompatible Transplants
After finding a suitable donor, it is crucial to ensure that the donor’s blood type is compatible with the recipient’s blood type. Incompatible transplants can lead to various risks and complications, including organ rejection and potentially life-threatening complications.
When a transplant recipient’s immune system recognizes the transplanted organ as foreign, it may attack and destroy the organ, causing organ rejection. Incompatible blood types are one of the most significant factors that increase the risk of organ rejection. For instance, if a person with blood type A receives an organ from a donor with blood type B, the recipient’s immune system will recognize the transplanted organ as foreign and attack it. This can lead to severe complications, including organ failure and death. Therefore, it is essential to perform blood typing tests before transplant surgery to ensure that the donor and recipient’s blood types are compatible.
Moreover, incompatible transplants can also cause other complications, such as infections, bleeding, and blood clots. These complications can arise due to the body’s immune response to the transplanted organ, which can trigger the formation of blood clots or cause bleeding. In some cases, infections can also occur due to the use of immunosuppressive drugs, which are used to prevent organ rejection. Therefore, it is crucial to monitor transplant recipients closely for any signs of complications and provide appropriate treatment promptly.
Overall, ensuring blood type compatibility is a crucial factor in reducing the risks and complications associated with transplantation.
Advances in Transplant Technology and Future Outlooks
Recent advancements in transplantation technology have opened up new possibilities for organ donation, including the use of bioengineering and regenerative medicine.
Bioengineering involves creating artificial organs or tissues in the laboratory, while regenerative medicine involves the use of stem cells to repair or replace damaged tissue.
Both of these approaches offer potential solutions to the shortage of donor organs, as they allow for the creation of new organs or tissues that can be transplanted into patients in need.
One of the key advantages of bioengineering and regenerative medicine is that they have the potential to eliminate the need for immunosuppressive drugs.
These drugs are currently used to prevent the body from rejecting transplanted organs, but they can have serious side effects and increase the risk of infections and cancer.
With bioengineered or regenerated organs, there is a lower risk of rejection since the organ is made from the patient’s own cells.
Additionally, these approaches could potentially reduce the waiting time for organ transplants, which can be a matter of life or death for some patients.
Overall, the future outlook for transplantation technology is promising, and continued research in this field could lead to significant improvements in patient outcomes.
Conclusion
In conclusion, blood typing and compatibility are crucial factors in transplant surgeries. Understanding the different blood types and antigens is essential for determining compatibility between a donor and a recipient. The Rh factor also plays a significant role in blood compatibility.
Cross-matching and testing for rejection are necessary steps in ensuring a successful transplant. Finding a suitable donor can be a challenging process, but with advances in technology, the process has become more manageable. Despite the risks and complications associated with incompatible transplants, the future outlook for transplant surgeries remains optimistic.
As technology continues to advance, the hope is that more patients will have access to compatible donors and successful transplant surgeries. Overall, blood typing and compatibility are vital aspects of the transplant process that cannot be overlooked.









