Bloodborne Pathogens: Protecting Yourself And Others
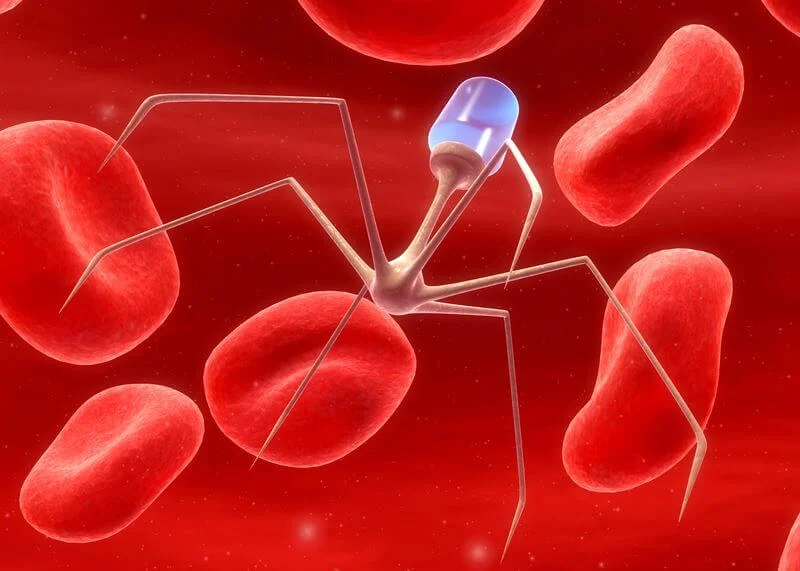
Bloodborne pathogens are microorganisms that are present in human blood and other bodily fluids. These pathogens can cause serious and often fatal illnesses such as HIV, hepatitis B and C, and other viral infections. Bloodborne pathogens are a significant occupational hazard for healthcare workers, as they are frequently exposed to potentially infectious materials.
As a result, it is vital for healthcare workers to understand the risks associated with bloodborne pathogens and take necessary precautions to protect themselves and others. This article aims to provide an overview of bloodborne pathogens, including:
- their types and transmission
- risks and precautions for healthcare workers
- safe handling and disposal of medical waste
- personal protective equipment and its proper use
- emergency response and exposure control plans
- prevention strategies for non-healthcare workers
- testing and treatment for bloodborne pathogens
- advocating for bloodborne pathogen awareness and education
By understanding the risks and taking necessary precautions, healthcare workers can protect themselves and their patients from the harmful effects of bloodborne pathogens.
Key Takeaways
- Healthcare workers are at risk of exposure to bloodborne pathogens and need to understand types and transmission modes to minimize infection risk.
- Use of personal protective equipment (PPE) and proper hand hygiene is necessary to prevent infection, but PPE is not a substitute for other infection control measures.
- Organizations must develop an exposure control plan to prevent pathogen spread and provide frequent PPE training for healthcare workers.
- Prevention strategies, such as personal protective equipment and good hygiene, should always be the first line of defense, and prompt testing and treatment can make a significant difference in health outcomes.
Understanding Bloodborne Pathogens: Types and Transmission
The recognition and understanding of the various types of bloodborne pathogens and their modes of transmission is crucial in order to adequately protect oneself and others from potential infection.
Bloodborne pathogens are microorganisms that are present in human blood and can cause disease in humans. They can be transmitted from one person to another through contact with infected blood or other body fluids such as semen, vaginal fluids, and breast milk.
The most commonly known bloodborne pathogens are hepatitis B, hepatitis C, and HIV. Hepatitis B is a viral infection that attacks the liver and can lead to chronic liver disease, liver cancer, and death.
Hepatitis C is another viral infection that affects the liver and can lead to cirrhosis and liver cancer. HIV is a viral infection that attacks the immune system and can lead to acquired immunodeficiency syndrome (AIDS).
Understanding the types and modes of transmission of bloodborne pathogens is essential in minimizing the risk of infection and ensuring the safety of oneself and others.
Risks and Precautions for Healthcare Workers
Healthcare workers face significant risks when dealing with infectious materials, thus necessitating the implementation of strict precautions to minimize the likelihood of infection transmission.
Bloodborne pathogens, including hepatitis B and C viruses and human immunodeficiency virus (HIV), can pose a serious threat to healthcare workers who come into contact with contaminated blood, bodily fluids, or other potentially infectious materials.
These pathogens can be transmitted through needlestick injuries, cuts, or exposure to mucous membranes, such as the eyes or mouth, and can lead to serious and potentially life-threatening infections.
To protect themselves and others from the risks of bloodborne pathogens, healthcare workers must follow strict precautions, including the use of personal protective equipment (PPE) such as gloves, gowns, and masks.
Proper hand hygiene is also crucial to prevent the spread of infection, and healthcare workers should wash their hands frequently and thoroughly with soap and water or use alcohol-based hand sanitizers.
In addition, healthcare workers should receive appropriate training on infection control measures and be aware of the specific risks associated with their job duties.
By taking these precautions, healthcare workers can minimize the risk of infection transmission and ensure the safety of themselves and their patients.
Safe Handling and Disposal of Medical Waste
Safe handling and disposal of medical waste is crucial in preventing the spread of infections and maintaining a clean and safe healthcare environment. Healthcare workers must be vigilant in their handling of medical waste to prevent accidental exposure to bloodborne pathogens. Additionally, proper disposal of medical waste is necessary to prevent contamination of the environment and potential harm to the general public.
One way to ensure safe handling and disposal of medical waste is to follow established protocols and guidelines. The following table outlines some of the general guidelines for handling and disposal of medical waste:
| Type of Waste | Handling Guidelines | Disposal Guidelines |
|---|---|---|
| Sharps (needles, blades, etc.) | Use puncture-resistant containers and never recap needles | Place in labeled, leak-proof containers and dispose of in designated sharps containers |
| Infectious waste (tissues, bodily fluids, etc.) | Use double-bagged containers and handle with gloves | Dispose of in labeled, leak-proof containers and incinerate or autoclave before disposal |
| Non-infectious waste (paper, plastic, etc.) | Use regular trash bags and handle with gloves | Dispose of in regular trash and follow local regulations for medical waste disposal |
By following these guidelines and properly handling and disposing of medical waste, healthcare workers can help prevent the spread of infections and protect themselves, their colleagues, and the general public.
Personal Protective Equipment (PPE) and Proper Use
Adhering to established protocols for the use of personal protective equipment (PPE) is critical in minimizing the risk of exposure to infectious agents during healthcare procedures. PPE serves as a barrier between the healthcare worker and the potentially infectious material, preventing direct contact or inhalation of harmful microorganisms.
The following are essential guidelines for the proper use of PPE:
- Choose the appropriate PPE based on the type of exposure and level of risk.
- Put on PPE before entering the patient’s room or handling equipment contaminated with infectious material.
- Remove PPE carefully to prevent contamination of skin or clothing.
- Dispose of used PPE according to institutional policies and regulations.
- Perform hand hygiene before and after wearing PPE.
It is important to note that the proper use of PPE is not a substitute for other infection control measures, such as hand hygiene and environmental cleaning. Instead, it should be viewed as an additional layer of protection that, when used correctly, can help prevent the spread of bloodborne pathogens and other infectious agents.
Healthcare workers should receive frequent training and education on the appropriate use of PPE to ensure their safety and that of their patients.
The use of personal protective equipment is an essential component of infection control in healthcare settings. Adhering to established protocols for the use of PPE can help minimize the risk of exposure to infectious agents during healthcare procedures. Healthcare workers should be trained and educated on the appropriate use of PPE and should follow institutional policies and regulations for its use and disposal.
Emergency Response and Exposure Control Plans
In emergency situations, having a well-designed response and exposure control plan is crucial in ensuring the safety of individuals and minimizing the spread of infectious agents.
Bloodborne pathogens can pose a serious threat to the health of individuals, and their exposure can occur in various settings, such as healthcare facilities, laboratories, and emergency response situations. Therefore, it is important for organizations to have an effective emergency response plan that includes procedures for identifying and addressing exposure incidents, as well as providing necessary medical treatment and follow-up care.
In addition to the emergency response plan, organizations must also develop an exposure control plan to prevent the spread of bloodborne pathogens. The exposure control plan should outline the measures to be taken to minimize the risk of exposure, such as the use of personal protective equipment, proper disposal of contaminated materials, and regular cleaning and disinfection of work areas.
Furthermore, it should provide training and education for employees on the risks associated with bloodborne pathogens, as well as the proper use of PPE and other control measures. By having a well-designed emergency response and exposure control plan, organizations can ensure the safety of their employees and prevent the spread of infectious agents.
Prevention Strategies for Non-Healthcare Workers
Preventing the transmission of infectious diseases outside of healthcare settings requires implementing effective strategies to minimize the risk of exposure. Non-healthcare workers should be aware of the potential risks associated with their work environment and be trained on how to properly handle and dispose of hazardous materials. Workers should also be provided with personal protective equipment such as gloves, masks, and gowns to reduce the risk of exposure.
In addition, workers should practice good hygiene, including regularly washing their hands with soap and water or using hand sanitizer. Workers should also avoid touching their face and mouth, especially when handling hazardous materials. Finally, workers should be educated on the signs and symptoms of infectious diseases, and be encouraged to seek medical attention if they experience any symptoms. By implementing these prevention strategies, non-healthcare workers can protect themselves and others from the transmission of infectious diseases.
| Column 1 | Column 2 | Column 3 |
|---|---|---|
| FACT | Bloodborne pathogens can lead to serious and potentially life-threatening infections. | |
| EMOTION | Fear of contracting a bloodborne pathogen can cause anxiety and stress. | |
| ACTION | Proper training and implementation of prevention strategies can reduce the risk of exposure and alleviate anxiety. | |
| RESULT | Workers can feel more confident and safe in their work environment, leading to increased productivity and job satisfaction. |
Testing and Treatment for Bloodborne Pathogens
Testing and treatment for infectious diseases can greatly improve the health outcomes of individuals who may have been exposed to hazardous materials in their work environment. It is important to note, however, that testing and treatment should not be viewed as a substitute for prevention strategies. Prevention strategies, such as using personal protective equipment and following proper infection control protocols, should always be the first line of defense against bloodborne pathogens.
In the event that an individual is exposed to a bloodborne pathogen, prompt testing and treatment can make a significant difference in their health outcomes. Testing can identify the specific pathogen and determine the appropriate treatment plan. Treatment may include antiviral medications or immunoglobulin therapy, depending on the pathogen and the severity of the infection.
It is important for individuals to seek medical attention immediately if they suspect they have been exposed to a bloodborne pathogen, as early detection and treatment can improve the likelihood of a successful outcome.
Advocating for Bloodborne Pathogen Awareness and Education
Advocacy efforts aimed at increasing awareness and education on the topic of preventing transmission of bloodborne diseases can be effective in promoting workplace safety and improving public health outcomes. By advocating for bloodborne pathogen awareness and education, individuals and organizations can help to reduce the risk of exposure to bloodborne pathogens, improve workplace safety, and ultimately, protect public health. This can be accomplished through a variety of means, including educational campaigns, training programs, and policy initiatives.
One effective strategy for advocating for bloodborne pathogen awareness and education is to provide individuals with the information and resources they need to protect themselves and others from exposure to bloodborne pathogens. This can involve educating individuals on the risks associated with bloodborne pathogens, as well as the steps they can take to prevent transmission. Other strategies may include lobbying for policy changes that promote workplace safety, partnering with other organizations to promote awareness and education, and using social media and other communication channels to spread the word about the importance of bloodborne pathogen awareness and education.
| Strategies | Benefits | Challenges | ||||
|---|---|---|---|---|---|---|
| Educational campaigns | Increase awareness, promote safety | May be costly, may not reach all individuals | ||||
| Training programs | Improve knowledge and skills, increase compliance | May be time-consuming, may be costly | ||||
| Policy initiatives | Improve workplace safety, promote compliance | May be difficult to implement, may face resistance | ||||
| Partnering with other organizations | Expand reach, increase resources | May be difficult to coordinate, may require compromise | ||||
| Social media and communication channels | Reach large audiences, raise awareness | May be difficult to control messaging, may not reach all individuals | Collaborating with experts in the field | Improve program effectiveness and credibility | May require additional resources and time for coordination |
Conclusion
In conclusion, understanding bloodborne pathogens and implementing safety measures to prevent their transmission is essential for both healthcare workers and the general public. Healthcare workers are at a higher risk of exposure due to their occupation, and it is crucial for them to follow proper protocols to protect themselves and their patients.
Safe handling and disposal of medical waste, use of personal protective equipment, and emergency response plans are all important aspects of preventing the spread of bloodborne pathogens in healthcare settings.
Non-healthcare workers also have a responsibility to educate themselves and take precautions to prevent the spread of bloodborne pathogens. This can include safe disposal of sharps and other medical waste, avoiding risky behaviors such as sharing needles, and getting tested for bloodborne pathogens if at risk.
By advocating for bloodborne pathogen awareness and education, we can work towards a safer and healthier community for all.