The Relationship Between Blood Pressure And Kidney Function
High blood pressure, also known as hypertension, is a common health condition that affects millions of people worldwide. It occurs when the force of blood against the walls of the arteries is too high, which can lead to serious health complications such as heart disease, stroke, and kidney damage.
In fact, hypertension is one of the leading causes of kidney disease, and understanding the relationship between blood pressure and kidney function is crucial for maintaining good health.
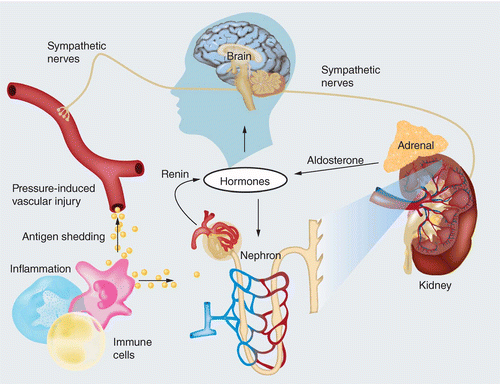
The kidneys play an important role in regulating blood pressure by filtering waste products and excess fluids from the blood. When the kidneys are functioning properly, they release a hormone called renin which helps to regulate blood pressure by constricting or dilating blood vessels.
However, when the kidneys are damaged, they may not be able to produce enough renin which can lead to high blood pressure. Additionally, high blood pressure can damage the blood vessels in the kidneys, which can lead to further kidney damage and a decline in kidney function over time.
This article will explore the relationship between blood pressure and kidney function, the causes and consequences of chronic kidney disease, and strategies for managing hypertension and maintaining healthy kidney function.
Key Takeaways
- High blood pressure can cause damage to the kidneys, leading to decreased renal function.
- Impairments in kidney function can lead to health problems such as hypertension, anemia, bone disease, and cardiovascular disease.
- Lifestyle modifications, pharmacological interventions, and close monitoring of renal function are necessary for effective management of hypertension and renal health.
- Regular physical activity, a healthy diet, and medication management are crucial for maintaining optimal blood pressure and renal function.
Understanding Hypertension and Its Impact on Health
The impact of hypertension on health is a critical area of study in understanding the relationship between blood pressure and kidney function, as it can lead to serious complications and long-term damage if left untreated.
Hypertension, also known as high blood pressure, occurs when the force of blood against the walls of arteries is consistently high. This can cause damage to the arteries and organs such as the kidneys, heart, and brain.
Hypertension is a major risk factor for kidney disease, as it can damage the blood vessels in the kidneys and reduce their ability to function properly.
When the kidneys are not functioning properly, they may not be able to remove waste and excess fluid from the body, which can lead to a buildup of toxins and fluid in the bloodstream. This can cause swelling in the legs, ankles, or feet, and can also lead to high blood pressure.
Therefore, it is important to manage hypertension to prevent long-term damage to the kidneys and other organs in the body.
The Importance of Kidney Function
Maintaining optimal health and well-being requires the efficient removal of waste and excess fluids from the body, which is primarily facilitated by the proper functioning of a vital organ responsible for filtration, balance, and regulation. This organ is none other than the kidney.
The kidney plays a crucial role in maintaining homeostasis by filtering waste products and excess fluids from the blood, regulating electrolyte balance, and producing hormones that control blood pressure and red blood cell production. Hence, the importance of kidney function cannot be overstated.
Impairments in kidney function can lead to a wide range of health problems, including hypertension, anemia, bone disease, and cardiovascular disease. The link between kidney function and blood pressure is particularly noteworthy.
High blood pressure, or hypertension, is a common condition that can damage the blood vessels and organs over time, including the kidneys. Conversely, kidney disease can also contribute to high blood pressure by disrupting the body’s ability to regulate fluid and sodium balance.
Therefore, it is essential to maintain healthy kidney function to prevent and manage hypertension and other associated health problems.
The Role of the Kidneys in Regulating Blood Pressure
Efficient filtration and regulation of fluid and electrolyte balance by a vital organ in the body is essential in controlling hypertension and related health problems. The kidneys play a significant role in regulating blood pressure by controlling the volume of blood and electrolytes in the body. Blood pressure is the force exerted by blood against the walls of blood vessels, and the kidneys regulate this pressure by controlling the amount of water and salt in the body.
The kidneys achieve this through various mechanisms, including the renin-angiotensin-aldosterone system (RAAS), which is activated when blood pressure drops. This system increases the production of the hormone aldosterone, which causes the kidneys to retain sodium and water, leading to an increase in blood volume and subsequently, blood pressure. Additionally, the kidneys produce a hormone called erythropoietin, which stimulates the production of red blood cells, helping to maintain blood volume and blood pressure. A summary of the kidney’s role in regulating blood pressure is presented in the table below.
| Mechanism | Description |
|---|---|
| RAAS | Activated when blood pressure drops, increases aldosterone production, causing the kidneys to retain sodium and water, leading to an increase in blood volume and subsequently, blood pressure. |
| Erythropoietin production | Stimulates the production of red blood cells, helping to maintain blood volume and blood pressure. |
The kidneys play a crucial role in regulating blood pressure by controlling the volume of blood and electrolytes in the body. Understanding the mechanisms through which the kidneys control blood pressure is essential in the management and treatment of hypertension and related health problems.
Chronic Kidney Disease and Its Causes
Chronic kidney disease, a progressive deterioration of renal function, can be caused by a variety of factors such as diabetes, hypertension, and autoimmune diseases. When the kidneys are damaged, they may not be able to filter waste and excess fluid from the blood properly. This can lead to a buildup of toxins in the body and cause other complications such as high blood pressure, anemia, and bone disease.
Diabetes is a major cause of chronic kidney disease, accounting for almost half of all cases. High blood sugar levels can damage the small blood vessels in the kidneys over time, leading to decreased kidney function.
Hypertension is another leading cause of chronic kidney disease. High blood pressure can damage the blood vessels in the kidneys and lead to a decrease in their ability to filter waste from the blood.
Other causes of chronic kidney disease include genetic factors, infections, and long-term use of certain medications. It is important to identify and manage these underlying causes to slow the progression of chronic kidney disease and prevent further kidney damage.
How High Blood Pressure Can Damage the Kidneys
High blood pressure, also known as hypertension, is a significant risk factor for chronic kidney disease (CKD). It can damage the small blood vessels in the kidneys that filter waste products from the blood. Over time, the damaged vessels can lead to decreased kidney function and even kidney failure. Hypertension can also cause proteinuria, a condition in which protein leaks into the urine, further damaging the kidneys.
CKD is a serious condition that can have long-term consequences, including an increased risk of heart disease and stroke. The mechanism by which high blood pressure damages the kidneys is not fully understood, but it is thought to involve changes in the structure and function of the blood vessels.
Hypertension can cause the blood vessels in the kidneys to narrow and become stiff, reducing blood flow to the kidneys. This can lead to ischemia, or a lack of oxygen and nutrients, which can cause the kidney tissue to die. Additionally, high blood pressure can increase the pressure within the glomeruli, which are the tiny filters in the kidneys that remove waste products from the blood. Over time, this increased pressure can damage the glomeruli and lead to proteinuria and decreased kidney function.
The Link Between Kidney Disease and High Blood Pressure
Recent research has shed light on the complex interplay between hypertension and renal health, revealing new insights into the pathogenesis and management of kidney disease. High blood pressure is a leading cause of kidney disease, and it is estimated that approximately 30% of adults with hypertension also have some degree of kidney damage.
The kidneys play a vital role in regulating blood pressure by filtering waste and excess fluid from the blood and maintaining a balance of electrolytes and fluid levels in the body. However, when blood pressure is consistently high, the delicate structures of the kidneys can become damaged, leading to a decline in kidney function.
The link between kidney disease and high blood pressure is bidirectional, with each condition exacerbating the other. As kidney function declines, blood pressure tends to rise, as the kidneys are less able to excrete excess fluid and maintain a healthy balance of electrolytes. Likewise, high blood pressure can cause damage to the blood vessels in the kidneys, reducing blood flow and causing scar tissue to form.
This can lead to a vicious cycle of declining kidney function and worsening hypertension. Effective management of hypertension is crucial in preventing and slowing the progression of kidney disease, and vice versa.
Managing Hypertension and Kidney Disease
Effective management of hypertension and renal health requires a comprehensive approach that includes lifestyle modifications, pharmacological interventions, and close monitoring of renal function. Lifestyle modifications such as dietary changes, exercise, and stress reduction can help control blood pressure and improve kidney function. Pharmacological interventions, such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), are commonly used to treat hypertension and can also have a beneficial effect on kidney function. It is important to closely monitor renal function in patients with hypertension, as the two conditions are closely linked and can exacerbate each other. Regular monitoring can allow for early detection and intervention, potentially preventing kidney damage and progression of hypertension.
To further illustrate the importance of managing hypertension and kidney disease, the following table outlines the recommended lifestyle modifications and pharmacological interventions for controlling blood pressure and improving renal health:
| Lifestyle Modifications | Pharmacological Interventions |
|---|---|
| DASH diet | ACE inhibitors |
| Regular exercise | ARBs |
| Stress reduction | Calcium channel blockers |
| Sodium restriction | Diuretics |
| Alcohol moderation | Beta blockers |
By implementing these lifestyle modifications and pharmacological interventions, patients with hypertension can improve their renal health and potentially prevent the development or progression of kidney disease. Close monitoring of renal function is also crucial in managing hypertension and kidney disease.
Strategies for Maintaining Healthy Blood Pressure and Kidney Function
One crucial aspect of maintaining overall health is through the implementation of strategies that promote optimal blood pressure and renal function. These strategies include regular physical activity, a healthy diet, and medication management.
Regular physical activity can help to lower blood pressure and improve renal function by improving overall cardiovascular health and reducing stress. A healthy diet that is low in sodium, saturated fats, and added sugars can also help to lower blood pressure and improve renal function. Additionally, it is important to carefully manage any medications prescribed for hypertension and kidney disease to ensure that they are effective and do not cause any adverse effects.
In addition to lifestyle changes and medication management, individuals with hypertension and kidney disease should also regularly monitor their blood pressure and kidney function. This can be done through regular check-ups with a healthcare provider and by tracking blood pressure and renal function at home. By regularly monitoring these measures, individuals can identify any changes or issues early on and work with their healthcare provider to address them before they become more serious.
Overall, implementing strategies that promote optimal blood pressure and renal function can have a significant impact on overall health and well-being, particularly for those with hypertension and kidney disease.
Conclusion
In conclusion, hypertension and kidney function are closely linked, with each impacting the other. The kidneys play a vital role in regulating blood pressure, and chronic kidney disease can lead to hypertension. Conversely, high blood pressure can damage the kidneys and contribute to the development of kidney disease.
Therefore, it is crucial to manage both conditions to maintain overall health. Strategies such as lifestyle modifications, medication management, and regular monitoring can help maintain healthy blood pressure and kidney function.
Further research is needed to better understand the relationship between these conditions and to develop effective prevention and treatment strategies. Overall, a comprehensive approach to managing hypertension and kidney disease is necessary to promote optimal health and well-being.