Diabetes Types And Metabolic Disorders Explained
Diabetes is a chronic metabolic disorder that affects millions of people worldwide. It is characterized by high blood glucose levels due to a deficiency in the hormone insulin, which regulates glucose uptake by cells in the body.
There are two main types of diabetes, type 1 and type 2, and several other metabolic disorders that affect blood sugar regulation. Understanding the different types of diabetes and their underlying causes is crucial for proper diagnosis and management of the condition.
This article will provide an overview of the different types of diabetes and metabolic disorders that affect blood sugar regulation. We will discuss the causes and symptoms of type 1 and type 2 diabetes, as well as the various treatment options available for each.
Additionally, we will explore other metabolic disorders that can affect glucose metabolism and discuss the long-term complications of diabetes and tips for prevention. By the end of this article, readers will have a better understanding of diabetes and its various forms, as well as the importance of proper management to prevent long-term complications.
Key Takeaways
- Diabetes is a chronic metabolic disorder that affects millions worldwide, with high blood glucose levels due to deficiency in hormone insulin.
- There are two main types of diabetes: type 1, caused by the destruction of insulin-producing beta cells in the pancreas, and type 2, with risk factors including genetic and environmental factors, obesity, and physical inactivity.
- Insulin therapy is critical for maintaining glucose homeostasis and preventing metabolic disorders, with different types of insulin available depending on individual factors.
- Long-term complications of high blood sugar levels can significantly impact overall health and quality of life, affecting various body systems including cardiovascular, nervous, and renal systems, but prevention is key to reducing the risk of developing long-term complications.
Understanding Insulin Regulation in the Body
Insulin regulation in the body involves the process of glucose uptake and utilization, which is mediated by insulin secretion and signaling pathways.
Insulin is a hormone secreted by the beta cells of the pancreas in response to rises in blood glucose levels.
Insulin secretion is stimulated by glucose entering the beta cells of the pancreas, which triggers the release of insulin from storage granules into the bloodstream.
The main function of insulin is to promote glucose uptake and utilization by the body’s cells, particularly in the liver, muscle, and adipose tissue.
Insulin binds to specific receptors on the surface of these cells, activating a signaling pathway that results in the transport of glucose from the bloodstream into the cells.
Insulin also stimulates the liver to convert excess glucose into glycogen, a storage form of glucose, and inhibits the breakdown of stored glycogen back into glucose.
Overall, insulin regulation is critical for maintaining glucose homeostasis in the body and preventing the development of metabolic disorders such as diabetes.
Type 1 Diabetes: Causes and Symptoms
One of the primary culprits behind the onset of Type 1 Diabetes is the destruction of insulin-producing beta cells in the pancreas. This autoimmune disease occurs when the body’s immune system attacks and destroys these cells, leaving the body unable to produce insulin. Without insulin, glucose cannot enter cells to provide energy, leading to high blood sugar levels and a range of symptoms.
The symptoms of Type 1 Diabetes can arise suddenly and may include frequent urination, increased thirst, extreme hunger, weight loss, fatigue, blurred vision, and irritability. It is important to recognize and treat these symptoms promptly, as untreated Type 1 Diabetes can lead to serious complications such as diabetic ketoacidosis, a potentially life-threatening condition.
While the exact cause of Type 1 Diabetes is unknown, it is thought to be related to genetic and environmental factors. Treatment typically involves insulin therapy, blood sugar monitoring, and lifestyle modifications.
Four common misconceptions about Type 1 Diabetes:
- Type 1 Diabetes is caused by eating too much sugar.
- Only children can develop Type 1 Diabetes.
- People with Type 1 Diabetes can’t eat any sugar or carbohydrates.
- Type 1 Diabetes can be cured by taking supplements or following a special diet.
Diagnosis and Treatment of Type 1 Diabetes
The proper diagnosis and treatment of Type 1 Diabetes involves a range of medical interventions and lifestyle modifications to manage blood sugar levels and prevent complications. The diagnostic process typically involves a combination of blood tests to measure glucose levels and antibodies that attack pancreatic cells responsible for producing insulin. Once a diagnosis is confirmed, treatment usually involves insulin therapy, which can be administered through injections or an insulin pump. Patients must also monitor their blood sugar levels regularly and make necessary adjustments to their insulin doses and diet to maintain stable glucose levels.
Table: Common Treatment Options for Type 1 Diabetes
| Treatment Option | Description | Pros | Cons | |||||
|---|---|---|---|---|---|---|---|---|
| Insulin Therapy | Administering insulin to regulate blood sugar levels | Effective at managing glucose levels | Requires careful monitoring and regular injections | |||||
| Continuous Glucose Monitoring | Using a device to track blood sugar levels in real-time | Provides constant monitoring and alerts to changes in glucose levels | Can be expensive and require frequent calibration | |||||
| Diet and Exercise | Making healthy food choices and engaging in physical activity to manage blood sugar levels | Can improve overall health and prevent complications | Requires significant lifestyle changes and may not be enough to control glucose levels alone | Medication and Insulin Therapy | May be necessary for individuals with type 1 diabetes or those with type 2 diabetes who cannot manage their blood sugar levels through lifestyle changes alone | Requires regular monitoring and careful dosing to prevent hypoglycemia or other complications | May be costly and require frequent doctor visits |
Type 2 Diabetes: Risk Factors and Prevention Strategies
Risk factors for developing Type 2 Diabetes include a combination of genetic and environmental factors. Obesity is a major risk factor for Type 2 Diabetes, as excess body fat can lead to insulin resistance and high blood sugar levels. Physical inactivity also increases the risk of developing Type 2 Diabetes, as regular exercise helps the body use insulin more effectively and maintain healthy blood sugar levels.
Family history of Type 2 Diabetes is another risk factor, as genetics can play a role in the development of the condition. Certain ethnicities, such as African Americans, Hispanic/Latino Americans, Native Americans, and Asian Americans, also have a higher risk of developing Type 2 Diabetes.
Prevention strategies for Type 2 Diabetes include maintaining a healthy weight, engaging in regular physical activity, and making healthy food choices. Studies have shown that losing just 5-7% of body weight and engaging in moderate-intensity physical activity for at least 150 minutes per week can significantly reduce the risk of developing Type 2 Diabetes.
Eating a balanced diet that is low in saturated and trans fats, added sugars, and sodium can also help prevent the condition. In addition, early screening and detection of pre-diabetes can help individuals make lifestyle changes to prevent the development of Type 2 Diabetes.
Lifestyle Changes for Managing Type 2 Diabetes
Effective management of Type 2 Diabetes requires consistent lifestyle changes that promote healthy blood sugar levels. These changes involve a combination of diet, exercise, and medication, and can be challenging for patients to implement. However, adopting healthy habits can significantly improve blood sugar control, reduce the risk of complications, and enhance overall quality of life.
To manage Type 2 Diabetes, patients should consider the following lifestyle changes:
- Diet modifications: Patients should aim to consume a balanced diet that is rich in whole grains, fruits, vegetables, lean proteins, and healthy fats. They should avoid sugary and processed foods, limit their intake of carbohydrates, and monitor portion sizes.
- Regular exercise: Physical activity can help improve insulin sensitivity, lower blood sugar levels, and reduce the risk of heart disease. Patients should aim to engage in moderate-intensity exercise for at least 30 minutes per day, five days a week.
- Medication adherence: Patients should take their prescribed medication as directed by their healthcare provider, and monitor their blood sugar levels regularly to ensure they are within the target range. They should also keep track of any side effects and report them to their healthcare provider.
Medications and Insulin Therapy for Type 2 Diabetes
Managing Type 2 Diabetes often requires the use of medications and insulin therapy in order to control blood sugar levels. There are several types of medications available to treat Type 2 Diabetes, including oral medications and injectable medications.
Oral medications work by stimulating the pancreas to produce more insulin, reducing the amount of glucose produced by the liver, and helping cells become more sensitive to insulin. Injectable medications work by mimicking the action of a hormone called incretin, which stimulates the pancreas to produce more insulin and slows down the rate at which the liver produces glucose.
Insulin therapy is often required when lifestyle changes and oral medications are not enough to control blood sugar levels. Insulin is a hormone that is produced by the pancreas and helps regulate blood sugar levels by allowing glucose to enter cells to be used as energy. In Type 2 Diabetes, the body either does not produce enough insulin or does not use it effectively.
Insulin therapy involves injecting insulin into the body to replace the missing or ineffective insulin. There are several types of insulin available, including rapid-acting, short-acting, intermediate-acting, and long-acting. The type of insulin used and the dosage will depend on the individual’s blood sugar levels and other factors such as weight, age, and overall health.
Other Metabolic Disorders that Affect Blood Sugar Regulation
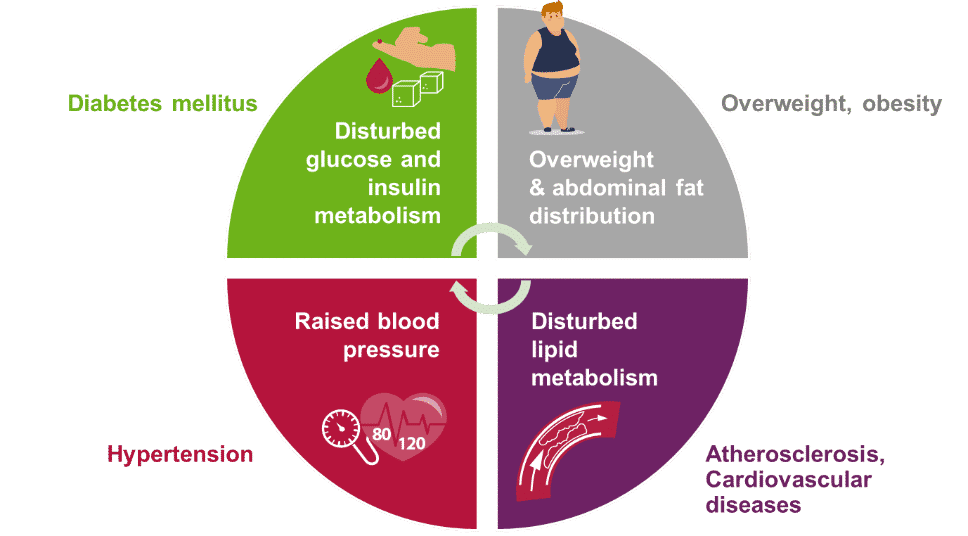
One important aspect of blood sugar regulation involves the balance between insulin and glucagon, two hormones that work together to maintain glucose homeostasis in the body. However, there are other metabolic disorders that can affect this delicate balance and lead to high or low blood sugar levels. Here are some examples:
- Cushing’s syndrome: This disorder is characterized by the overproduction of cortisol, a hormone that can increase blood sugar levels. People with Cushing’s syndrome may experience symptoms such as weight gain, high blood pressure, and muscle weakness.
- Hypothyroidism: When the thyroid gland doesn’t produce enough hormones, it can lead to a condition called hypothyroidism. This can affect blood sugar regulation because thyroid hormones play a role in insulin sensitivity. People with hypothyroidism may experience symptoms such as fatigue, weight gain, and depression.
- Acromegaly: This disorder is caused by an excess of growth hormone, which can lead to insulin resistance and high blood sugar levels. People with acromegaly may experience symptoms such as enlarged hands and feet, joint pain, and sleep apnea.
- Addison’s disease: This rare disorder occurs when the adrenal glands don’t produce enough hormones, including cortisol. This can lead to low blood sugar levels and other symptoms such as fatigue, muscle weakness, and weight loss.
Understanding these and other metabolic disorders is important for healthcare professionals who work with patients with diabetes or other conditions that affect blood sugar regulation. By identifying and treating these disorders, doctors can help their patients achieve better glucose control and prevent complications associated with high or low blood sugar levels.
Long-Term Complications of Diabetes and Prevention Tips
The long-term complications of high blood sugar levels can significantly impact a person’s overall health and quality of life. Diabetes is a chronic condition that affects various body systems, including the cardiovascular, nervous, and renal systems. The risk of developing complications increases with the length of time a person has diabetes and the severity of their blood sugar control. Some of the most common complications include neuropathy, retinopathy, nephropathy, and cardiovascular disease.
Prevention is the key to reducing the risk of developing long-term complications. Managing blood sugar levels through medication, diet, and exercise can help prevent or delay complications. Regular monitoring of blood pressure and cholesterol levels is also essential in preventing cardiovascular disease. Quitting smoking and maintaining a healthy weight are additional lifestyle changes that can help reduce the risk of complications. Overall, it is crucial for individuals with diabetes to work closely with their healthcare team to develop a comprehensive plan for managing their condition and reducing the risk of long-term complications.
| Complication | Description |
|---|---|
| Neuropathy | Nerve damage that can cause pain, numbness, or tingling in the extremities |
| Retinopathy | Damage to the blood vessels in the eyes that can lead to vision loss |
| Nephropathy | Kidney damage that can progress to kidney failure |
| Cardiovascular Disease | Increased risk of heart attack, stroke, and peripheral artery disease |
This table highlights some of the most common complications of diabetes, which can evoke emotions in the audience. The description of each complication can help readers understand the impact that high blood sugar levels can have on the body. Providing concrete examples of the potential consequences of uncontrolled diabetes can motivate individuals to take action to prevent complications.
Conclusion
In conclusion, diabetes and other metabolic disorders are complex conditions that require a thorough understanding of insulin regulation in the body.
Type 1 diabetes is caused by an autoimmune response that destroys insulin-producing cells, while type 2 diabetes is often associated with lifestyle factors such as obesity and sedentary behavior.
Effective management of diabetes involves a combination of lifestyle changes and medication or insulin therapy.
Prevention strategies for type 2 diabetes include maintaining a healthy weight, exercising regularly, and eating a balanced diet.
It is also important to monitor blood sugar levels, and to seek medical attention if symptoms of diabetes or other metabolic disorders arise.
By taking proactive steps to manage these conditions, individuals can reduce their risk of long-term complications and improve their overall health and wellbeing.