The Fascinating World Of Blood Transfusion: History And Modern Practices
Blood transfusion is a vital component of modern medicine and has played a significant role in saving countless lives over the years. The practice of blood transfusion dates back to the early 17th century, where the first documented experiments involved animal-to-human transfusions. Over the years, blood transfusion has evolved significantly, with advancements in technology and medical knowledge leading to safer and more efficient transfusions.
This article aims to explore the fascinating world of blood transfusion, tracing its history from early experiments to modern practices. We will delve into the discovery of blood types, cross-matching, and the development of safer transfusions.
Additionally, we will examine the common uses and indications for transfusions, the latest advancements in technology, and ethical and safety considerations in transfusion practice. This article offers an in-depth look at the importance of blood transfusion in modern medicine and highlights the significant advancements made in this field over the years.
Key Takeaways
- The discovery of blood types, particularly ABO and Rh systems, revolutionized transfusion practices and increased safety.
- Ethical and safety considerations are crucial in blood transfusion practice.
- Uses of blood transfusion include emergency care, surgery, and treatment of chronic medical conditions.
- Technological innovations, such as nucleic acid testing and specialized blood products, have increased safety and efficiency in transfusion practices.
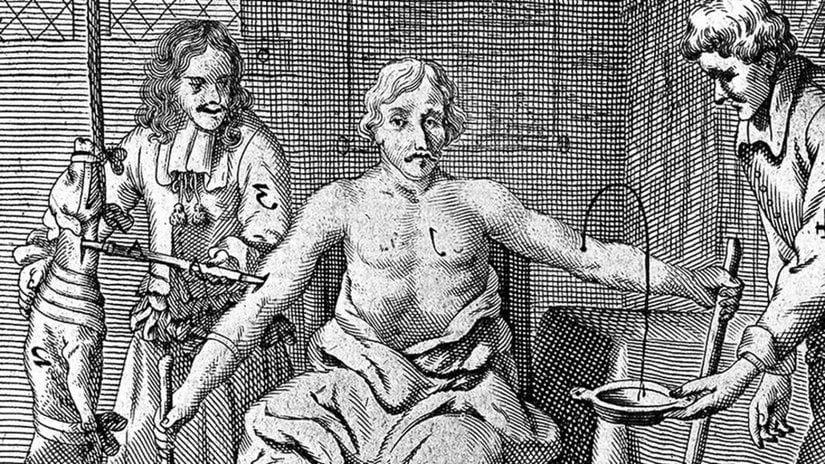
Early Experiments with Blood Transfusion
In the early stages of blood transfusion experimentation, physicians utilized a variety of animal blood types with varying degrees of success and complications. The first recorded blood transfusion was performed in the 17th century by a British physician, Richard Lower, who successfully transfused blood from a sheep to a human. However, subsequent attempts were not always successful, and many patients died as a result of complications such as blood clots and immune reactions.
The 19th century saw significant progress in the field of blood transfusion, with the discovery of blood typing and the development of techniques for preserving and storing blood. In 1901, Austrian physician Karl Landsteiner identified the ABO blood groups, which paved the way for safe and successful blood transfusions. Blood typing allowed physicians to determine the compatibility of blood types between donor and recipient, reducing the risk of adverse reactions and increasing the success rate of transfusions.
Today, blood transfusions are a routine medical procedure, with millions of transfusions performed each year to treat a wide range of conditions, from anemia to cancer.
Animal-to-Human Transfusions and Early Risks
Animal-to-human transfusions were attempted in the early days of blood transfusion, but posed significant risks due to the incompatibility between animal and human blood. The first documented animal-to-human transfusion was performed by Richard Lower in 1665, who successfully transfused sheep blood into a human, but the patient died shortly after.
Similarly, in 1667, Jean-Baptiste Denis transfused calf blood into a young man, who also died soon after. These early experiments underscored the need for compatibility testing prior to transfusion and led to the development of blood typing and cross-matching techniques.
The early attempts at animal-to-human transfusions highlight the desperation and lack of understanding surrounding blood transfusions at the time, and the risks that patients were willing to take to find a cure.
The tragic outcomes of these early experiments underscore the importance of safety and compatibility testing in medical procedures, and the need for thorough research and development before introducing new treatments.
Despite the risks and failures of early animal-to-human transfusions, the experimentation paved the way for the development of modern blood transfusion practices, which have saved countless lives and continue to be a vital component of modern medicine.
The Discovery of Blood Types
The discovery of different blood types has revolutionized the field of medicine, allowing for safer and more effective transfusions that have saved countless lives. The existence of distinct blood types was first hypothesized in the early 20th century, but it was not until the work of Karl Landsteiner in 1901 that their existence was definitively proven. Landsteiner discovered that when he mixed blood samples from different individuals, some would clump together, while others would not. He identified three distinct blood types, which he labeled A, B, and O. Later, a fourth blood type, AB, was discovered by another researcher.
Today, we know that there are actually over 30 different blood groups, each with their own unique characteristics. These blood groups are determined by the presence or absence of specific proteins, called antigens, on the surface of red blood cells. The most important blood groups for transfusion purposes are the ABO and Rh systems, which are used to match donors and recipients to minimize the risk of adverse reactions. The following table provides an overview of the different blood types and their associated antigens:
| Blood Type | Antigens Present on Red Blood Cells | Can Donate to | Can Receive from |
|---|---|---|---|
| A | A antigen | A, AB | A, O |
| B | B antigen | B, AB | B, O |
| AB | A and B antigens | AB only | A, B, AB, O |
| O | Neither A nor B antigens | A, B, AB, O | O only |
The discovery of blood types and the subsequent development of safe transfusion practices has saved countless lives and transformed the field of medicine. Today, blood transfusions are routine procedures that are used to treat a wide range of conditions, from trauma to leukemia. However, despite these advances, there is still a need for ongoing research to improve transfusion safety and efficacy, particularly in the face of emerging infectious diseases and changing demographics.
Cross-Matching and Safer Transfusions
Cross-matching techniques have been developed to minimize the risk of adverse reactions during blood transfusions by ensuring compatibility between the donor and recipient.
Cross-matching refers to the process of testing the donor’s blood against the recipient’s blood to detect any incompatibilities.
This is done by mixing the donor’s blood with the recipient’s blood and observing the reaction.
If the two blood types are incompatible, the recipient’s immune system may attack and destroy the donor’s red blood cells, leading to a transfusion reaction.
Cross-matching is typically done before the transfusion to prevent any adverse reactions.
There are two main techniques used for cross-matching: the indirect antiglobulin test (IAT) and the immediate spin cross-matching.
The IAT involves mixing the donor’s blood with the recipient’s plasma, while the immediate spin cross-matching involves mixing the donor’s blood with the recipient’s red blood cells.
Both techniques are used to detect any antibodies that may cause a transfusion reaction.
Cross-matching is an essential step in blood transfusion, as it helps ensure that the recipient receives the correct blood type and minimizes the risk of adverse reactions.
Blood Transfusions in Modern Medicine
Advancements in technology and medical practices have significantly improved the safety and effectiveness of blood transfusions in modern medicine. Blood transfusion is a critical life-saving procedure that involves the transfer of blood or blood components from a donor to a recipient. The procedure is used to treat various medical conditions such as severe bleeding, anemia, and blood disorders. However, blood transfusions can also pose several risks, including transfusion reactions, infections, and transfusion-related acute lung injury (TRALI).
To reduce the risks associated with blood transfusions, modern medical practices have implemented several safety measures. One of the essential safety measures is the screening of blood donors for infectious diseases such as HIV, hepatitis B and C, and syphilis. Transfusion medicine specialists also perform pre-transfusion testing, including cross-matching and antibody screening, to ensure compatibility between the donor and recipient blood. Moreover, modern technology has made it possible to produce blood components that are safer and more effective. For instance, blood products such as platelets, red blood cells, and plasma can now be processed and stored for extended periods, ensuring a readily available supply for patients in need.
| Blood Component | Uses | Shelf Life (days) |
|---|---|---|
| Red Blood Cells | Treat anemia, severe bleeding | 42 |
| Platelets | Treat bleeding disorders, cancer | 5 |
| Plasma | Treat clotting disorders, burns, shock | 365 |
| Cryoprecipitate | Treat clotting disorders | 1 year |
The table above illustrates the different blood components and their uses, as well as their shelf life. Blood banks and transfusion centers use these blood components to provide patients with the necessary treatment. By implementing these safety measures and utilizing modern technology, blood transfusions have become a safer and more reliable medical procedure for patients in need.
Common Uses and Indications for Transfusion
Blood transfusions have become an essential aspect of modern medicine. They are used in a variety of medical settings, including emergency care, surgery, and treatment of chronic medical conditions. In the previous subtopic, we explored the history of blood transfusions in modern medicine. In this section, we will discuss the common uses and indications for transfusion.
One of the primary indications for blood transfusion is to replace blood loss due to injury or surgery. This is particularly important in emergency situations where rapid blood loss can lead to shock and even death. In such cases, transfusions are used to restore blood volume and prevent complications.
Additionally, patients undergoing major surgeries may require transfusions to replace blood lost during the procedure. Blood transfusions are also used in the treatment of chronic conditions such as anemia, which can occur due to a variety of reasons such as chronic kidney disease, cancer, or other illnesses. In these cases, transfusions are used to replace red blood cells and improve oxygenation of the body.
Another common indication for blood transfusion is in the treatment of certain cancers, such as leukemia and lymphoma. Chemotherapy and radiation therapy can damage bone marrow, which is responsible for producing blood cells. In such cases, transfusions are used to restore blood cell counts and prevent complications such as infections and bleeding.
Finally, blood transfusions are used in some rare genetic disorders such as sickle cell anemia and thalassemia, which can cause chronic anemia. In these cases, transfusions are used to replace the abnormal red blood cells with healthy ones, reducing symptoms and improving quality of life.
Overall, blood transfusions are a vital tool in modern medicine, providing life-saving treatments to millions of patients every year.
Advancements in Blood Transfusion Technology
In recent years, technological innovations have greatly improved the safety and efficacy of transfusions in medical practice.
One of the most significant advancements in blood transfusion technology is the use of nucleic acid testing (NAT) to screen donated blood for infectious diseases. NAT can detect the genetic material of viruses, such as HIV and hepatitis C, in the blood of donors, even before they produce antibodies. This allows blood banks to identify and discard infected donations before they are used for transfusions, greatly reducing the risk of transmitting these diseases to patients.
Another important advancement in blood transfusion technology is the use of leukoreduction filters to remove white blood cells from donated blood. White blood cells can cause adverse reactions in some patients, such as fevers, chills, and lung damage. Leukoreduction filters can also reduce the risk of transfusion-related infections and improve the shelf life of blood products.
Other technological improvements include automated blood collection and processing systems, which increase the safety and efficiency of blood transfusions, and the development of specialized blood products, such as frozen plasma and cryoprecipitate, which can be used to treat specific medical conditions.
Overall, these advancements have greatly improved the safety and effectiveness of blood transfusions, making them an essential tool in modern medical practice.
Ethical and Safety Considerations in Blood Transfusion Practice
Ethical considerations regarding blood transfusions include issues related to informed consent, patient autonomy, and the allocation of scarce resources. Informed consent is a crucial aspect of blood transfusion practice, as patients need to be fully informed about the risks and benefits of the transfusion before they can make an informed decision about whether or not to receive it. This can be challenging, particularly in emergency situations where patients may not be in a position to give their consent.
Additionally, some patients may refuse blood transfusions due to religious or personal beliefs, which can pose a challenge for healthcare providers who are trying to ensure that their patients receive the best possible care. To ensure that ethical considerations are taken into account, healthcare providers must carefully weigh the risks and benefits of blood transfusions for each individual patient. This includes considering factors such as the patient’s age, medical history, and the specific medical conditions that they are being treated for.
Healthcare providers must also take steps to minimize the risk of complications associated with blood transfusions, such as infection or allergic reactions. To achieve this, they may use special filters or perform pre-transfusion testing to ensure that the patient’s blood is compatible with the donor blood.
Overall, ethical and safety considerations are crucial in blood transfusion practice, and healthcare providers must take great care to ensure that patients receive the best possible care while also respecting their rights and autonomy.
- Factors to consider when weighing the risks and benefits of blood transfusions include the patient’s age, medical history, and specific medical conditions.
- Informed consent is crucial in blood transfusion practice, but can be challenging in emergency situations or when patients refuse transfusions due to religious or personal beliefs.
- Healthcare providers must take steps to minimize the risk of complications associated with blood transfusions, such as infection or allergic reactions.
- Special filters or pre-transfusion testing may be used to ensure that the patient’s blood is compatible with the donor blood.
- Ethical and safety considerations are crucial in blood transfusion practice, and healthcare providers must take great care to ensure that patients receive the best possible care while also respecting their rights and autonomy.
Conclusion
In conclusion, blood transfusion is a fascinating world that has evolved over time from early experiments to modern practices.
Animal-to-human transfusions and early risks led to the discovery of blood types which made cross-matching and safer transfusions possible.
Today, blood transfusions are used for a variety of indications, and advancements in technology have made it easier to obtain and process blood products.
Despite the advancements, ethical and safety considerations remain crucial in blood transfusion practice.
Healthcare professionals must ensure that patients receive the correct blood products and take necessary measures to prevent transfusion reactions.
Moreover, blood banks must adhere to strict regulations and screening procedures to prevent the transmission of infections.
It is evident that blood transfusion is a complex field that requires collaboration between various stakeholders to ensure safe and effective transfusion practices.