What Are Antineoplastic Medications And How Do They Target Cancerous Cells?

This article aims to provide an overview of antineoplastic medications and their mechanisms of action in targeting cancerous cells.
Cancer, a complex disease characterized by uncontrolled cell growth and proliferation, is a major global health concern. Antineoplastic medications, also known as anticancer or chemotherapy drugs, have been developed to specifically inhibit or destroy cancer cells, thereby preventing their further growth and spread.
Understanding the underlying mechanisms by which these medications exert their therapeutic effects is crucial for optimizing treatment strategies and improving patient outcomes.
This article will explore the different mechanisms of action employed by antineoplastic medications, including their ability to interfere with cellular processes essential for cancer cell survival and proliferation.
Additionally, the article will discuss the various methods of administration, common side effects, treatment plans, and dosages, as well as potential future developments and ongoing research in the field of antineoplastic medication therapy.
Key Takeaways
- Antineoplastic medications are drugs used to treat cancer.
- Combination therapies, which involve using multiple drugs to target cancer cells, can enhance treatment effectiveness and reduce drug resistance.
- Targeted therapies, such as monoclonal antibodies, tyrosine kinase inhibitors, and PARP inhibitors, focus on specific proteins or enzymes involved in cancer cell growth and division.
- Emerging treatments like immune checkpoint inhibitors, CAR-T cell therapy, and cancer vaccines offer new hope and improved outcomes in cancer treatment.
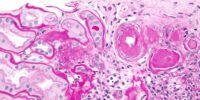
Understanding Cancer Cells
Cancer cells, characterized by uncontrolled growth and division, present a formidable challenge in terms of their ability to evade normal regulatory mechanisms and spread throughout the body.
Understanding the mechanisms behind cancer cell growth is crucial for developing effective antineoplastic medications. Cancer cells acquire unique genetic mutations that enable them to proliferate uncontrollably and survive in adverse conditions. These mutations can occur due to various factors, including exposure to carcinogens, genetic predisposition, or errors during DNA replication.
Mutations in key genes involved in cell cycle regulation, DNA repair, and apoptosis contribute to the uncontrolled growth of cancer cells. Antineoplastic medications aim to target these specific genetic mutations, inhibiting the pathways that drive cancer cell growth and division.
By targeting the unique vulnerabilities of cancer cells, these medications can effectively impede their growth and spread, leading to improved patient outcomes.
Introduction to Antineoplastic Medications
Characterized by their ability to inhibit the growth and division of malignant cells, these therapeutic agents play a pivotal role in the treatment of various neoplastic diseases. Antineoplastic medications, commonly referred to as chemotherapy drugs, are a key component of cancer treatment.
These medications target cancerous cells through different mechanisms, allowing for effective control and elimination of tumors.
- DNA damage: Antineoplastic medications can cause DNA damage in cancer cells, preventing them from replicating and dividing.
- Cell cycle disruption: These medications can disrupt the cell cycle of cancer cells, preventing them from progressing through the different stages of cell division.
- Apoptosis induction: Some antineoplastic medications can trigger apoptosis, a programmed cell death mechanism, in cancer cells.
- Angiogenesis inhibition: Certain medications can inhibit the formation of new blood vessels, cutting off the blood supply to tumors and hindering their growth.
By targeting specific aspects of cancer cell biology, antineoplastic medications provide an effective means to treat neoplastic diseases and improve patient outcomes.
Mechanisms of Action
This paragraph will introduce the discussion on the mechanisms of action of antineoplastic medications.
Antineoplastic medications are designed to target cancer cells specifically, while sparing normal cells. They achieve this by interfering with key processes involved in cell division and DNA replication, which are crucial for the growth and survival of cancer cells.
By disrupting these processes, antineoplastic medications can effectively inhibit the proliferation of cancer cells and ultimately lead to their death.
How antineoplastic medications target cancer cells
Antineoplastic medications selectively target cancer cells by interfering with specific molecular pathways essential for their growth and survival. These medications are designed to interact with the unique characteristics of cancer cells, taking advantage of their vulnerabilities while minimizing harm to healthy cells.
One way antineoplastic medications achieve this selectivity is by targeting proteins that are overexpressed or mutated in cancer cells. By binding to these proteins, the medications can disrupt crucial signaling pathways, leading to cell cycle arrest, DNA damage, or apoptosis.
Additionally, antineoplastic medications can also interfere with the tumor microenvironment, inhibiting angiogenesis or modulating the immune response against cancer cells.
While these medications are effective, cancer cells can develop resistance mechanisms that render them less susceptible to their effects. Therefore, combination therapies and ongoing research are essential to overcome resistance and improve patient outcomes.
Interference with cell division and DNA replication
Interference with cell division and DNA replication disrupts the growth and proliferation of cancer cells, leading to potential therapeutic benefits. Antineoplastic medications target cancerous cells by interfering with the cell cycle regulation and DNA repair mechanisms.
This disruption can occur through different mechanisms, such as inhibiting specific enzymes involved in DNA replication or preventing the formation of microtubules required for cell division. By targeting these processes, antineoplastic medications induce DNA damage and inhibit cell division, thereby inhibiting the growth of cancer cells.
Strategies used by these medications include:
- Inhibition of DNA polymerase enzymes
- Disruption of microtubule formation
- Promotion of DNA damage
- Inhibition of DNA repair mechanisms
- Induction of apoptosis
These strategies aim to selectively target cancer cells while minimizing damage to healthy cells, as cancer cells often have dysregulated cell cycle control and impaired DNA repair mechanisms.
By interfering with cell division and DNA replication, antineoplastic medications offer potential therapeutic benefits in the treatment of cancer.
Administration Methods
One effective way to administer antineoplastic medications is through intravenous infusion, allowing for precise dosing and rapid distribution throughout the body.
Intravenous administration involves injecting the medication directly into a vein, either as a bolus or through a continuous infusion. This method offers several advantages, including the ability to quickly deliver high concentrations of the medication and adjust the dosage as needed.
Additionally, intravenous infusion allows for the administration of larger volumes of medication compared to other routes, such as oral or intramuscular administration.
However, there are also dosage considerations to take into account when administering antineoplastic medications intravenously. Factors such as the patient’s body surface area, renal function, and overall health status need to be considered to ensure the appropriate dosage is administered to maximize efficacy while minimizing toxicity.
Common Side Effects
A notable consequence of antineoplastic medication administration is the occurrence of common side effects. These medications, while effective in targeting cancer cells, can also affect healthy cells in the body, leading to various adverse reactions. Some common side effects include nausea, vomiting, fatigue, hair loss, and decreased immune function. Additionally, antineoplastic medications can have long-term effects on the body, such as organ damage and increased risk of secondary cancers. Another concern is the development of drug resistance, which occurs when cancer cells adapt and become resistant to the effects of the medication. This can limit the effectiveness of antineoplastic drugs and pose challenges in treating cancer. It is essential for healthcare professionals to carefully monitor and manage these side effects to ensure the best possible outcomes for patients.
| Side Effects | Long-Term Effects | Drug Resistance |
|---|---|---|
| Nausea | Organ damage | Development |
| Vomiting | Secondary cancers | of resistance |
| Fatigue | Increased risk | |
| Hair loss | ||
| Decreased immune function |
Treatment Plans and Dosages
Antineoplastic medications are crucial in the treatment of cancer, as they specifically target cancerous cells and impede their growth and division. However, alongside their therapeutic benefits, these medications are associated with a range of side effects that can vary depending on the specific drug and individual patient characteristics.
Moving forward to the current subtopic, it is imperative to consider treatment plans and dosages. Determining the appropriate treatment plan and dosage for each patient is essential to maximize the effectiveness of antineoplastic medications. Healthcare professionals carefully assess factors such as the type and stage of cancer, the patient’s overall health, and potential drug interactions to devise an individualized treatment strategy.
In some cases, alternative therapies may be explored to complement conventional antineoplastic medications and potentially enhance treatment outcomes. These alternative therapies can include targeted therapies, immunotherapies, or participation in clinical trials.
Combination Therapies
Combination therapies involving different treatment modalities are frequently employed in cancer management to optimize treatment outcomes and address the complexities of the disease.
Cancer cells can develop resistance to antineoplastic medications, leading to treatment failure. Combination therapies aim to overcome this drug resistance by targeting multiple pathways involved in cancer cell survival and proliferation.
By using a combination of drugs that act on different targets, it is possible to enhance the effectiveness of treatment and reduce the likelihood of resistance development.
Additionally, combination therapies can have synergistic effects, where the combination of drugs produces a greater effect than the sum of their individual effects. This approach allows for a more comprehensive and targeted attack on cancerous cells, increasing the likelihood of successful treatment outcomes.
However, the selection of drugs and dosages in combination therapies must be carefully considered to minimize toxicity and side effects.
Future Developments and Research
This paragraph discusses future developments and research in the field of cancer treatment.
It focuses on advancements in targeted therapies, emerging treatments, and potential breakthroughs.
These areas of research are crucial for improving the effectiveness and precision of cancer treatments and offer hope for better outcomes for patients.
By exploring new ways to target cancer cells and developing innovative therapies, scientists aim to revolutionize cancer treatment and ultimately improve the prognosis for individuals with cancer.
Advancements in targeted therapies
Significant progress has been made in the field of cancer treatment with the development of targeted therapies that selectively attack cancer cells while sparing healthy ones. This has led to advancements in immunotherapy and personalized medicine in cancer treatment. Immunotherapy utilizes the body’s immune system to fight against cancer cells. It involves the use of substances that either stimulate the immune system or enhance its ability to recognize and destroy cancer cells. Personalized medicine, on the other hand, tailors treatment to an individual’s specific genetic makeup and the characteristics of their cancer. This approach allows for more effective and precise treatment, minimizing the side effects often associated with traditional chemotherapy. The following table showcases some examples of targeted therapies in cancer treatment:
| Targeted Therapy | Mechanism of Action |
|---|---|
| Monoclonal antibodies | Bind to specific proteins on cancer cells, inhibiting their growth and promoting immune responses against them. |
| Tyrosine kinase inhibitors | Block the activity of specific enzymes involved in cancer cell growth and division. |
| PARP inhibitors | Inhibit the activity of an enzyme called PARP, which plays a role in DNA repair. By blocking this enzyme, cancer cells are unable to repair DNA damage and ultimately die. |
| Checkpoint inhibitors | Block proteins that regulate immune responses, allowing the immune system to recognize and attack cancer cells more effectively. |
These advancements in targeted therapies have revolutionized cancer treatment, offering new hope for patients and improving outcomes. Further research and development in this field hold great promise for the future of cancer treatment.
Emerging treatments and potential breakthroughs
Emerging treatments and potential breakthroughs in cancer research are paving the way for innovative approaches that hold immense promise in transforming the landscape of cancer treatment.
One area of focus is the development of potential immunotherapies, which aim to harness the body’s immune system to target and destroy cancer cells. These therapies involve the use of various agents, such as immune checkpoint inhibitors, CAR-T cell therapy, and cancer vaccines. These treatments have shown remarkable efficacy in certain types of cancer, leading to durable responses and improved survival rates for patients.
Additionally, alternative treatment approaches are being explored, including targeted therapies that exploit specific genetic mutations in cancer cells and the development of novel drug delivery systems.
With continued research and advancements in these areas, there is hope that these emerging treatments will provide new options for patients and ultimately improve outcomes in cancer treatment.
Frequently Asked Questions
Are there any natural alternatives to antineoplastic medications?
Natural alternatives to antineoplastic medications exist, but their efficacy in comparison to conventional treatments is not well-established. Further research is needed to determine their potential as alternative options for cancer treatment.
Can antineoplastic medications be used to treat all types of cancer?
Antineoplastic medications are not effective for all types of cancer. While they are the standard treatment, alternative treatments may be considered due to the limitations of antineoplastic medications in targeting all cancer cells.
What precautions should be taken when handling antineoplastic medications?
Precautions must be taken when handling antineoplastic medications. These include wearing appropriate protective equipment, such as gloves and gowns, and following proper procedures for handling, administration, and disposal to minimize the risk of exposure and potential adverse effects.
Are there any long-term side effects of antineoplastic medications?
Long-term effects of antineoplastic medications may include organ damage, infertility, and increased risk of secondary cancers. Alternatives to antineoplastic medications include targeted therapies, immunotherapies, and alternative treatments such as herbal remedies or acupuncture.
How does the cost of antineoplastic medications impact patient access to treatment?
The cost implications of antineoplastic medications pose affordability challenges for patients, potentially limiting their access to treatment. This financial burden can hinder the ability of individuals to receive necessary cancer therapies.